When people go under cardiac arrest, stroke, or any other health condition that causes them not to breathe properly or deprives them of oxygen, do you know what doctors do to help them breathe?
In such situations like that, there are various techniques and equipment that people use to help a person who is unable to breathe get oxygen in his/her system. These could range from the popular mouth-to-mouth resuscitation which can be used to revive a fainted person to the use of breathing equipment for mechanical ventilation like the oxygen pump.
What is normally used in hospitals and clinics to keep oxygen-deprived patients going or alive are breathing equipments used for mechanical ventilation, and this is the focus of this article today.
This post will explain all you need to know about mechanical ventilation; how it’s done, when it’s the best time for it, and the precautions to note about it, as well as other dos and don’ts about mechanical ventilation.
Alright, enough intro. Let’s get down to business.
What is Mechanical Ventilation?
Mechanical ventilation is a kind of life support that allows you to breathe when you are unable to do so on your own. This may happen during surgery or when you’re really ill.
While mechanical ventilation cannot cure diseases directly, it may keep you stable while other therapies and drugs help your body heal. Mechanical ventilation is a sort of treatment that assists you in breathing or breaths for you when you are unable to do so on your own.[mfn]https://my.clevelandclinic.org/health/treatments/15368-mechanical-ventilation[/mfn].
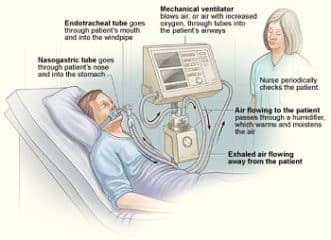
You may be placed on a ventilator during a surgical operation or if your lungs are not functioning correctly. Mechanical ventilation keeps the airways open while also delivering oxygen and removing carbon dioxide. The patient underwent image guided bronchoscopy to investigate a suspicious lesion in their lung.
What Exactly is a Ventilator?
A ventilator is a machine that assists you in breathing. The ventilator, like crutches, either partly or entirely supports your lung functions.
The functions of a ventilation system include the following:
- It delivers oxygen to your lungs.
- Aids in the removal of carbon dioxide (CO2) from the lungs.
- Provides pressure to protect the little air sacs (alveoli) in your lungs from collapsing.
- Providers may modify the machine’s settings to match your individual requirements.
Watch the video below to know about mechanical ventilation:
What Exactly is the Difference Between Intubation and Mechanical Ventilation?
Intubation and mechanical ventilation are often used simultaneously, however, they are not the same thing. A provider intubates you by inserting a tube down your mouth into your airway (trachea). The tube in your neck will then be connected to a ventilator by a provider. You may not need to be intubated if a face mask links you to the ventilator.
Types of Ventilation
Positive pressure Ventilation
The design of the modern positive-pressure ventilators was based mainly on technical developments by the military during World War II to supply oxygen to fighter pilots at high altitudes. Such ventilators replaced the iron lungs as safe endotracheal tubes with high-volume/low-pressure cuffs were developed.
The popularity of positive-pressure ventilators rose during the polio epidemic in the 1950s in Scandinavia and the United States and was the beginning of modern ventilation therapy.
Positive pressure through a manual supply of 50% oxygen through a tracheostomy tube led to a reduced mortality rate among patients with polio and respiratory paralysis. However, because of the sheer amount of manpower required for such manual intervention, mechanical positive-pressure ventilators became increasingly popular.
Positive-pressure ventilators work by increasing the patient’s airway pressure through an endotracheal or tracheostomy tube. The positive pressure allows air to flow into the airway until the ventilator breath is terminated. Then, the airway pressure drops to zero, and the elastic recoil of the chest wall and lungs push the tidal volume — the breath out through passive exhalation.
Negative pressure ventilation
Negative pressure mechanical ventilators are produced in small, field-type, and larger formats. The prominent design of the smaller devices is known as the cuirass, a shell-like unit used to create negative pressure only to the chest using a combination of a fitting shell and a soft bladder.
In recent years this device has been manufactured using various-sized polycarbonate shells with multiple seals, and a high-pressure oscillation pump in order to carry out biphasic cuirass ventilation.
Its main use has been in patients with neuromuscular disorders that have some residual muscular function. The latter, larger formats are in use, notably with the polio wing hospitals in England such as St Thomas’ Hospital in London and the John Radcliffe in Oxford.
The larger units have their origin in the iron lung, also known as the Drinker and Shaw tank, which was developed in 1928 by J.H Emerson Company and was one of the first negative-pressure machines used for long-term ventilation. It was refined and used in the 20th century largely as a result of the polio epidemic that struck the world in the 1940s. The machine is, in effect, a large elongated tank, which encases the patient up to the neck.
The neck is sealed with a rubber gasket so that the patient’s face (and airway) are exposed to the room air. While the exchange of oxygen and carbon dioxide between the bloodstream and the pulmonary airspace works by diffusion and requires no external work, air must be moved into and out of the lungs to make it available to the gas exchange process.
In spontaneous breathing, a negative pressure is created in the pleural cavity by the muscles of respiration, and the resulting gradient between the atmospheric pressure and the pressure inside the thorax generates a flow of air. In the iron lung by means of a pump, the air is withdrawn mechanically to produce a vacuum inside the tank, thus creating negative pressure.[mfn]https://emedicine.medscape.com/article/304068-overview[/mfn]
This negative pressure leads to the expansion of the chest, which causes a decrease in intrapulmonary pressure and increases the flow of ambient air into the lungs. As the vacuum is released, the pressure inside the tank equalizes to that of the ambient pressure, and the elastic recoil of the chest and lungs leads to passive exhalation.
However, when the vacuum is created, the abdomen also expands along with the lung, cutting off venous flow back to the heart, and leading to the pooling of venous blood in the lower extremities. The patients can talk and eat normally and can see the world through a well-placed series of mirrors. Some could remain in these iron lungs for years at a time quite successfully.
Some of the problems with the full body design were such as being unable to control the inspiratory to expiratory ratio and the flow rate. This design also caused blood to pool in the legs.
Intermittent abdominal pressure ventilation
Another type is the intermittent abdominal pressure ventilator which applies pressure externally via an inflated bladder, forcing exhalation, sometimes termed exsufflation. The first such apparatus was the Bragg-Paul Pulsator. The name of one such device, the Pneumobelt made by Puritan Bennett has to a degree become a generic name for the type.
Oscillator ventilation
The most commonly used high-frequency ventilator and the only one approved in the United States is the 3100A from Vyaire Medical. It works by using very small tidal volumes by setting the amplitude and a high rate set in hertz. This type of ventilation is primarily used for neonates and pediatric patients who are failing conventional ventilation.
High-Frequency Jet Ventilation
The first type of high-frequency ventilator is made for neonates and is the only jet type is made by Bunnell Incorporated. It works in conjunction with a separate CMV ventilator to add pulses of air to the control breaths and PEEP.
What are the Different Types of Mechanical Ventilation?
Ventilators come in many different styles and methods of giving a breath to sustain life. There are manual ventilators such as bag valve masks and anesthesia bags that require the users to hold the ventilator to the face or to an artificial airway and maintain breaths with their hands.
Mechanical ventilators are ventilators not requiring operator effort and are typically computer-controlled or pneumatic-controlled. Mechanical ventilators typically require power from a battery or a wall outlet (DC or AC) though some ventilators work on a pneumatic system not requiring power.
There are a variety of technologies available for ventilation, falling into two main (and then lesser categories), the two being the older technology of negative-pressure mechanisms, and the more common positive-pressure types.
Common positive-pressure mechanical ventilators include:
- Transport ventilators: These ventilators are small and more rugged, and can be powered pneumatically or via AC or DC power sources.
- Intensive-care ventilators: These ventilators are larger and usually run on AC power (though virtually all contain a battery to facilitate intra-facility transport and as a backup in the event of a power failure). This style of ventilator often provides greater control of a wide variety of ventilation parameters (such as inspiratory rise time). Many ICU ventilators also incorporate graphics to provide visual feedback on each breath.
- Neonatal ventilators (bubble CPAP, HFJV, HFOV): Designed with the preterm neonate in mind, these are a specialized subset of ICU ventilators that are designed to deliver smaller volumes and pressures to these patients. These may be conventional or high-frequency types.
- Positive airway pressure ventilators (PAP): These ventilators are specifically designed for non-invasive ventilation. This includes ventilators for use at home for treatment of chronic conditions such as sleep apnea or COPD and in the ICU setting. Positive pressure is used in modern mechanical ventilators to force air into your lungs. Positive pressure ventilation is available in the following types:
- Invasive mechanical ventilation: A tube in your airway is attached to a ventilator. This tube may be inserted via your mouth (intubation) or your neck (tracheostomy).
- Noninvasive ventilation: A face mask attached to a ventilator is used. Straps attach the mask on your head to keep it in place. Air is pushed into your lungs by the ventilator. Noninvasive ventilation systems such as CPAP or BiPAP are examples of noninvasive ventilation.
What is the Purpose of Mechanical Ventilators?
When you are unable to breathe on your own, providers employ mechanical ventilators to assist you.
Ventilation using mechanical means:
- Provision of oxygen for the patient.
- Removal of excess carbon dioxide so that it does not accumulate.
- Stopping sections of the lungs from collapsing due to a lack of pressure.
Who Needs Mechanical Ventilation?
You may need mechanical respiration:
- During a surgical operation: General anesthesia might make it difficult to breathe normally.
- If you have any of the following lung diseases or infections.
- If you are in a medical emergency because anything can clog your airway making breathing difficult.
- If you have brain injuries or disorders: Your brain may not communicate well with the rest of your body, especially your lungs, preventing you from breathing normally.
- If you have any disorders that cause your blood to contain too much carbon dioxide (hypercapnia) or insufficient oxygen (hypoxia).
- To prevent fluids from unintentionally entering your lungs (aspiration).
Specific situations that may need mechanical ventilation include:
- The syndrome of acute respiratory distress (ARDS)
- Pneumonia
- COVID-19, as well as other respiratory disorders.
- Obstructive pulmonary disease (COPD)
- Stroke
- Traumatic brain damage
- Coma
- Anaphylaxis
How Long Can Someone be Kept on a Mechanical Ventilator?
The duration of mechanical ventilation is determined by the cause.[mfn]https://en.wikipedia.org/wiki/Mechanical_ventilation[/mfn] It might be years, months, weeks, days, or even hours. You should only be on a ventilator for as little time as feasible. Your health providers will assess your capacity to breathe on your own on a daily or more frequent basis.
Generally, if you must be on a ventilator for an extended period of time (two weeks or more), your provider will move you from an endotracheal tube to a neck tube (tracheostomy).
How is Invasive Mechanical Ventilation Done?
A provider will initiate invasive mechanical ventilation by:
- Giving you sedative drugs to calm you and keep you from moving (paralytic). You’ll most likely be sedated throughout the duration of the procedure, but the paralytic will wear off once you’re on the ventilator.
- Inserting an endotracheal tube (ET) into your neck and trachea (airway leading to your lungs).
- Connecting the tubing to the ventilator. The ventilator will assist you in breathing until your medical team determines that it is safe for you to do it again.
These are the general procedures for kicking off mechanical ventilation. Some of these measures may alter depending on your personal scenario, particularly whether or not it is an emergency.
The Breath Delivery Mechanisms Involved in Mechanical Ventilation
- Trigger: The trigger, either flow or pressure, is what causes a breath to be delivered by a mechanical ventilator. Breaths may be triggered by a patient taking their own breath, a ventilator operator pressing a manual breath button, or based on the set respiratory rate.
- Cycle: The cycle is what causes the breath to transition from the inspiratory phase to the exhalation phase. Breaths may be cycled by a mechanical ventilator when a set time has been reached, or when a preset flow or percentage of the maximum flow delivered during a breath is reached depending on the breath type and the settings. Breaths can also be cycled when an alarm condition such as a high-pressure limit has been reached.
- Limit: Limit is how the breath is controlled. Breaths may be limited to a set maximum pressure or volume.
- Breath exhalation: Exhalation in mechanical ventilation is almost always completely passive. The ventilator’s expiratory valve is opened, and expiratory flow is allowed until the baseline pressure (PEEP) is reached. Expiratory flow is determined by patient factors such as compliance and resistance.
Various Procedures and Materials Related to a Mechanical Ventilator
There are various procedures and mechanical devices that provide protection against airway collapse, air leakage, and aspiration:
- Face mask — In resuscitation and for minor procedures under anesthesia, a face mask is often sufficient to achieve a seal against air leakage. Airway patency of the unconscious patient is maintained either by manipulation of the jaw or by the use of the nasopharyngeal or oropharyngeal airway. These are designed to provide a passage of air to the pharynx through the nose or mouth, respectively. Poorly fitted masks often cause nasal bridge ulcers, a problem for some patients. Face masks are also used for non-invasive ventilation in conscious patients. A full-face mask does not, however, provide protection against aspiration. Non-invasive ventilation can be considered for epidemics of COVID-19 where sufficient invasive ventilation capacity is not available (or in some milder cases), but pressurized protection suits for caregivers are recommended due to the risks of poorly fitting masks emitting contaminating aerosols.
- Tracheal intubation is often performed for mechanical ventilation of hours to weeks duration. A tube is inserted through the nose (nasotracheal intubation) or mouth (orotracheal intubation) and advanced into the trachea. In most cases, tubes with inflatable cuffs are used for protection against leakage and aspiration. Intubation with a cuffed tube is thought to provide the best protection against aspiration. Tracheal tubes inevitably cause pain and coughing. Therefore, unless a patient is unconscious or anesthetized for other reasons, sedative drugs are usually given to provide tolerance to the tube. Other disadvantages of tracheal intubation include damage to the mucosal lining of the nasopharynx or oropharynx and subglottic stenosis.
- Supraglottic airway — a supraglottic airway (SGA) is any airway device that is seated above and outside the trachea, as an alternative to endotracheal intubation. Most devices work via masks or cuffs that inflate to isolate the trachea for oxygen delivery. Newer devices feature esophageal ports for suctioning or ports for tube exchange to allow intubation. Supraglottic airways differ primarily from tracheal intubation in that they do not prevent aspiration. After the introduction of the laryngeal mask airway (LMA) in 1998, supraglottic airway devices have become mainstream in both elective and emergency anesthesia. There are many types of SGAs available including the esophageal-tracheal combitube (ETC), laryngeal tube (LT), and the obsolete esophageal obturator airway (EOA).
- Cricothyrotomy — Patients requiring emergency airway management, in whom tracheal intubation has been unsuccessful, may require an airway inserted through a surgical opening in the cricothyroid membrane. This is similar to a tracheostomy but a cricothyrotomy is reserved for emergency access.
- Tracheostomy — When patients require mechanical ventilation for several weeks, a tracheostomy may provide the most suitable access to the trachea. A tracheostomy is a surgically created passage into the trachea. Tracheostomy tubes are well tolerated and often do not necessitate any use of sedative drugs. Tracheostomy tubes may be inserted early during treatment in patients with pre-existing severe respiratory disease, or in any patient expected to be difficult to wean from mechanical ventilation, i.e., patients with little muscular reserve.
- Mouthpiece — Less common interface, does not provide protection against aspiration. There are lip-seal mouthpieces with flanges to help hold them in place if a patient is unable.
What Happens When You’re on a Breathing Machine?
Providers will undertake additional treatments to treat you or avoid problems while you are on a ventilator.
These are some examples:
- Monitoring: Your provider will hook you up to other equipment that will monitor how your body works. This involves keeping track of your:
- Blood pressure
- Heart rate
- Respiration rate (how many breaths you take per minute).
- Levels of oxygen
They may also use chest X-rays to examine your lungs or blood tests to measure your oxygen and carbon dioxide levels.
- Suctioning: Suctioning is necessary to keep your airways clean. A catheter (a thin tube) will be inserted into the breathing tube by a provider to assist in the removal of mucus (secretions). It may cause you to cough or gag. It may be upsetting for loved ones to witness.
- Medications: Your doctor may provide aerosolized (spray) drugs via your breathing tube. These drugs operate best when inhaled directly into the airways or lungs. Your doctor will also inject drugs into your veins through an IV
- Nutrition: You are unable to eat or drink normally when on a ventilator and intubated. Your provider will provide liquid nourishment to you, often through a tube that passes through your nostrils and into your stomach. Fluids will be administered via an IV in a vein.
- Mobilization: Your service providers will call you on a frequent basis. They may sometimes get you up and moving.
- Bronchoscopy: Bronchoscopy is used by doctors to examine the airways in your lungs. They introduce a tiny, illuminated camera into your lungs through the breathing tube. They may collect mucus or tissue samples for examination at times.
When You’re on a Ventilator, Who Looks after You?
When you need mechanical ventilation, you are treated in the critical care unit (ICU). They may keep a tight eye on you there. All ICU personnel are highly educated to care for patients who need mechanical breathing.
Providers that may be able to help you include:
- Therapists who work with the lungs
- Anesthesiologists, pulmonologists, and critical care doctors
- Nurse practitioners
- Registered nurses
- Nurse aides
Are you Conscious When on a Mechanical Ventilator?
Your provider will aim to keep you as alert as possible while keeping you quiet and comfortable while you’re on a ventilator. They will utilize drugs to keep you calm as required. You may be awake (conscious), yet you may feel drowsy, disoriented, or not entirely aware of what is going on.
Depending on your condition, your provider may need to keep you thoroughly sedated (asleep) so you won’t be conscious and your body can recuperate. To prevent you from injuring yourself by tugging on the tube, your arms may be restrained.
What Happens If You Stop using Mechanical Ventilation?
Before pulling you off the ventilator, providers will do tests to check whether you can breathe on your own. For these examinations, the ET tube remains in place.
When your condition has stabilized and you are able to breathe unaided, your provider will withdraw the ET tube and you will no longer need mechanical ventilation.
After your physician removes the ET tube, you may have a painful throat or mouth, or your voice may become raspy.
Your provider may put you on various devices to help you breathe after removing the tube (called extubation). Oxygen masks or noninvasive ventilation (with a mask) are examples of this. A provider may need to re-intubate you and put you back on mechanical ventilation.
What are the Benefits of Mechanical Ventilation?
Mechanical ventilation has the following advantages:
- Breathing does not need any effort.
- Your body can concentrate on recovering from infections or other ailments.
- It supplies all of the oxygen you need while also removing carbon dioxide.
- It generates pressure to protect your lungs’ tiny sacs from collapsing.
- It keeps your lungs open.
What are the Hazards Associated with Mechanical Ventilation?
Mechanical ventilation difficulties are avoided by providers.
However, there may be some hazards, such as:
- Infections caused by bacteria: Bacteria may enter your lungs via the tube in your airways, causing diseases such as ventilator-associated pneumonia (VAP). Antibiotics are used to treat this.
- Damage to the lungs: The ventilator’s pressure might harm your lungs.
- Lung Collapse: If a section of your lung becomes weak, it may create a hole, causing your lungs to collapse (pneumothorax).
- Changes in the heart and blood flow: Being on a ventilator might have an impact on how your heart operates. If your heart isn’t working properly, it might lower your blood pressure or increase your heart rate. These alterations may also result in less oxygen reaching your blood (decreased perfusion), despite the fact that plenty is reaching your lungs.
- People are sometimes unable to take off a ventilator: If you need to be on a ventilator for an extended period of time, your tube will be removed from your mouth. A tube will be inserted via a tiny cut (incision) in your neck.
- Extending the dying process: If someone’s health is unlikely to improve, placing them on mechanical ventilation may help them die. This may result in unneeded pain. In this scenario, your provider will advise you on mechanical ventilation options.
Advanced Complications of Mechanical Ventilation
Complications can occur at any stage of mechanical ventilation and are sometimes life-threatening. Complications that can occur during the placement of an endotracheal tube include upper airway and nasal trauma, tooth avulsion, oral-pharyngeal laceration, laceration or hematoma of the vocal cords, tracheal laceration, perforation, hypoxemia, and intubation of the esophagus.
Below are advanced complications of mechanical ventilation:
1. Ventilator-induced lung injury
With a ventilator-induced lung injury, the alveolar epithelium is at risk for both barotrauma and volutrauma:
- Barotrauma
Barotrauma refers to the rupture of the alveolus with the subsequent entry of air into the pleural space (pneumothorax) and/or the tracking or air along the vascular bundle to the mediastinum (pneumomediastinum).
The true prevalence of barotrauma is difficult to establish, but reports suggest a rate of 10%. Large tidal volumes (> 10 mL/kg) and elevated peak inspiratory and plateau pressures (Pplat > 35) are the most important risk factors.
Studies in patients with adult respiratory distress syndrome (ARDS) demonstrated that the severity of the underlying lung pathology is a better predictor of barotrauma than the observed peak inspiratory pressure. Even so, peak inspiratory pressures of less than 45 cm water and plateau pressures of less than 30-35 cm water are recommended.
The inspiratory-to-expiratory ratio can be adjusted by increasing the inspiratory flow rate, decreasing the tidal volume, and by decreasing the ventilatory rate. Attention to the inspiratory-to-expiratory ratio is important to prevent barotrauma in patients with obstructive airway disease (eg, asthma and chronic obstructive pulmonary disease).
Management of barotrauma includes addressing specific complications (eg, chest tube for pneumothorax), lowering plateau pressure to less than 30 by reducing tidal volume and PEEP, and managing the underlying disorder. Barotrauma may be associated with increased mortality, although it is often not the direct cause of death.
- Volutrauma
Volutrauma refers to the local overdistention of normal alveoli. Volutrauma has gained recognition over the last 2 decades and is the impetus for lung protective ventilation with lower tidal volumes of 6–8 mL/kg.
Computed tomography scans have demonstrated that ARDS has a heterogeneous pattern of lung involvement. The abnormal consolidated lung is dispersed within normal lung tissue. When a mechanical ventilation breath is forced into the patient, the positive pressure tends to follow the path of least resistance to the normal or relatively normal alveoli, potentially causing overdistention.
This overdistention sets off an inflammatory cascade that augments or perpetuates the initial lung injury, causing additional damage to previously unaffected alveoli. The increased local inflammation lowers the patient’s potential to recover from ARDS.
The inflammatory cascade occurs locally and may augment the systemic inflammatory response as well. Thus, it is possible to develop this atelectrauma without high tidal volumes, indicating the need to have a high index of suspicion for this complication.
Another aspect of volutrauma associated with positive ventilation is the shear force associated with the opening and closing effects on collapsible alveoli. This has also been linked to worsening the local inflammatory cascade.
PEEP prevents the alveoli from totally collapsing at the end of exhalation and may be beneficial in preventing this type of injury. Since volutrauma was recognized, a lung-protective ventilation strategy is recommended in all patients with ARDS or acute lung injury. Of note, lung-protective ventilation has not been shown to decrease mortality or other outcomes in non-ARDS mechanically ventilated patients.
2. Oxygen Toxicity
Oxygen toxicity is a function of increased FIO2 and its duration of use. Oxygen toxicity is due to the production of oxygen-free radicals, such as superoxide anion, hydroxyl radical, and hydrogen peroxide. Oxygen toxicity can cause a variety of complications ranging from mild tracheobronchitis and absorptive atelectasis to diffuse alveolar damage that is indistinguishable from ARDS.
No consensus has been established for the level of FIO2 required to cause oxygen toxicity, but this complication has been reported in patients given a maintenance FIO2 of 50% or greater. The clinician is encouraged to use the lowest FIO2 that accomplishes satisfactory oxygenation.
The medical literature suggests that the clinician should attempt to attain an FIO2 of 60% or less within the first 24 hours of mechanical ventilation. If necessary, PEEP should be considered a means to improve oxygenation while a safe FIO2 is maintained. When PEEP is effective and not contraindicated because of hemodynamics or other reasons, the patient can usually be oxygenated while the risks of oxygen toxicity are limited.
3. Ventilator-associated pneumonia
Ventilator-associated pneumonia (VAP) is a life-threatening complication with mortality rates of 33-50%. It is reported to occur in 8-28% of patients given mechanical ventilation. The incidence is 1-4 cases per 1000 ventilator days.
The risk of VAP is highest immediately after intubation. VAP is estimated to occur at a rate of 3% per day for the first 5 days, 2% per day for the next 5 days, and 1% per day thereafter. VAP occurs more frequently in trauma, neurosurgical, or burn units than in respiratory units and medical intensive care units.
VAP is defined as a new infection of the lung parenchyma that develops within 48 hours after intubation. The diagnosis can be challenging. VAP should be suspected when a new or changing pulmonary infiltrate is seen in conjunction with fever, leukocytosis, and purulent tracheobronchial secretions. However, many diseases can cause this clinical scenario.
Examples include aspiration pneumonitis, atelectasis, pulmonary thromboembolism, drug reactions, pulmonary hemorrhage, and radiation-induced pneumonitis. Qualitative and quantitative cultures of protected brush and bronchoalveolar lavage specimens may help with the diagnosis, but the utility of these techniques is still debated.
Microorganisms implicated in VAP that occur in the first 48 hours after intubation are flora of the upper airway, including Haemophilus influenza and Streptococcus pneumonia. After this early period, gram-negative bacilli such as Pseudomonas aeruginosa; Escherichia coli; and Acinetobacter, Proteus, and Klebsiella species predominate.
Staphylococcus aureus, especially methicillin-resistant S aureus (MRSA), typically becomes a major infective agent after 7 days of intubation and mechanical ventilation. Most of the medical literature recommends initial therapy with broad-spectrum antibiotics that cover pathogens resistant to multiple drugs until the sensitivities of the causative organism are identified.
Knowledge of organisms that cause VAP in the individual ICU and the pattern of antibiotic resistance is imperative. Choices of antibiotics should be tailored to the microorganisms and the antimicrobial resistance observed in each ICU. It is important to use an infection-prevention bundle to prevent VAP.
One such bundle can be remembered by the mnemonic I COUGH. I is for incentive spirometry; C is for cough and deep breathing; O is for oral care; U is for understanding; G is for getting out of bed; H is for the head of the bed elevation.
4. Intrinsic PEEP, or auto-PEEP
Intrinsic positive end-expiratory pressure (PEEP) or auto-PEEP is a complication of mechanical ventilation that most frequently occurs in patients with COPD or asthma who require a prolonged expiratory phase of respiration. These patients may have difficulty in totally exhaling the ventilator-delivered tidal volume before the next machine breath is delivered.
When this problem occurs, a portion of each subsequent tidal volume may be retained in the patient’s lungs, a phenomenon sometimes referred to as breath stacking (see image below). If this goes unrecognized, the patient’s peak airway pressure may increase to a level that results in barotrauma, volutrauma, hypotension, patient-ventilator dyssynchrony, or death.
Manometry performed by using an esophageal balloon to record changes in pleural pressure is the most accurate way to recognize intrinsic PEEP. However, this technology is not available at most institutions. Therefore, clinicians must anticipate this complication and carefully monitor the measured peak airway pressure.
When intrinsic PEEP is diagnosed, the patient should temporarily be released from mechanical ventilation to allow for full expiration. The ventilator can then be adjusted to shorten inspiration by decreasing the set tidal volume, increasing the inspiratory flow rate, or reducing the frequency of respiration.
These maneuvers, if performed properly, can increase the expiratory time. The normal inspiratory to the expiratory ratio (I:E ratio) is 1:2. In patients with obstructive airway disease, the target I:E ratio should be 1:3 to 1:4.
5. Cardiovascular effects
Mechanical ventilation always has some effect on the cardiovascular system. Positive-pressure ventilation can decrease preload, stroke volume, and cardiac output. Positive-pressure ventilation also affects renal blood flow and function, resulting in gradual fluid retention.
The incidence of stress ulcers and sedation-related ileus is increased when patients receive mechanical ventilation. In fact, mechanical ventilation is a primary indication for GI prophylaxis. Positive pressure maintained in the chest may decrease venous return from the head, increasing intracranial pressure and worsening agitation, delirium, and sleep deprivation.
How Long Does Mechanical Ventilation Take to Recover From?
The length of time it takes you to recover from mechanical ventilation is determined by why you need it and how long you were on it. Your physician will be able to inform you what to anticipate and how to care for yourself as you heal.
Alternative Modes of Mechanical Ventilation
In the last 2 decades, several modes of ventilation have emerged from the successful merging of ventilator and computer technologies. Staying abreast of emerging ventilator modifications can be a formidable and ongoing challenge for physicians.
Dual-control ventilation modes were designed to combine the advantages of volume-control ventilation (guaranteed minute ventilation) with pressure-control ventilation (rapid, variable flow at a preset or limited peak airway pressure).
These dual-control modes attempt to increase the safety and comfort of mechanical ventilation. Although these new technologies seem promising, no findings from randomized trials indicate improved patient outcomes (including mortality).
Dual-control, breath-to-breath, pressure-limited, time-cycled ventilation
This mode has been called pressure-regulated volume-control (PRVC), adaptive pressure ventilation, auto-flow, volume-control plus, or variable-pressure control ventilation according to various commercial ventilators. This mode is under the dual control of pressure and volume.
The physician presets a desired tidal volume, and the ventilator delivers a pressure-limited (controlled) breath until that preset tidal volume is achieved. The breath is essentially like a conventional pressure-controlled ventilation breath, but the ventilator can guarantee a predetermined minute of ventilation.
Breath to breath, the inspiratory pressure is automatically adjusted down or up according to the patient’s lung compliance and/or resistance to deliver a preset tidal volume. The ventilator monitors each breath and compares the delivered tidal volume with the set tidal volume.
If the delivered volume is too low, it increases the inspiratory pressure on the next breath. If it is too high, it decreases the inspiratory pressure to the next breath. This adjustment gives the patient the lowest peak inspiratory pressure needed to achieve a preset tidal volume. The advantage of this mode is that it gives the physician the opportunity to deliver a minimum minute ventilation at the lowest peak airway pressure possible.
Dual-control breath-to-breath, pressure-limited, flow-cycled ventilation
This mode has been called volume-support ventilation (VSV) or variable-pressure-support according to which ventilator is used. This mode is a combination of pressure support ventilation (PSV) and volume-control ventilation. Like PSV, the patient triggers every breath, controlling his or her own respiratory frequency and inspiratory time.
This mode delivers a breath exactly like conventional PSV, but the ventilator can guarantee minute ventilation. The pressure support is automatically adjusted up or down according to the patient’s lung compliance and/or resistance to deliver a preset tidal volume.
This mode is similar to the dual-control breath-to-breath, pressure-limited, time-cycled ventilation except that it is flow-cycled, which means that the patient determines the respiratory rate and inspiratory time. The mode cannot be used in a patient who lacks spontaneous breathing effort.
Volume support has also been marketed as a self-weaning mode. Therefore, as the patient’s effort and/or compliance or resistance improve, pressure support is automatically titrated down without the need for input from a physician or therapist.
A number of potential problems can arise. If the patient’s metabolic demand increases, and raises the tidal volume, the pressure support decreases to provide less ventilatory support when the patient needs it most. The clinician must be aware that, as the level of pressure support drops, mean airway pressure decreases. This effect may result in hypoxemia.
The other concern is that the tidal volume must be correctly set to the patient’s metabolic needs. If the tidal volume is set too high, weaning is delayed. If it is set too low, the work of breathing may be more than what the patient can reasonably accomplish.
Automode and variable support or variable-pressure control
This mode is basically the combination of the 2 modes described above. If the patient has no spontaneous breaths, the ventilator is set up in PRVC mode. However, when the patient takes 2 consecutive breaths, the mode is switched to VSV. If the patient becomes apneic for 12 seconds, the ventilator switches back to PRVC mode.
Automode and variable support or variable-pressure control were designed for automatic weaning from pressure control to pressure support depending on the patient’s effort. This ventilatory mode can also be used in conventional volume control and volume support.
Again, the mode depends on the patient’s effort. To the authors’ knowledge, no randomized trials have been conducted to evaluate this auto-mode, and no evidence suggests that this type of weaning is more effective than conventional weaning.
Dual control within a breath
This mode has been called volume-assured pressure support or pressure augmentation according to various manufacturers. This mode can switch from pressure control to volume control within a single specific breath cycle. After a breath is triggered, rapid and variable flow creates pressure to reach the set level of pressure support.
The tidal volume that is delivered from the machine is monitored. If the tidal volume equals the minimum set tidal volume, the patient receives a typical pressure-supported breath, which makes this mode essentially like volume support. However, if the tidal volume is less than the set tidal volume, the ventilator switches to a volume-controlled breath with constant flow rate until the set tidal volume is reached.
One study compared volume-assured pressure support with simple assist-control volume support and showed a 50% reduction in the work of breathing, lowered airway resistance, and lowered intrinsic PEEP. However, because of its complexity, this mode is rarely used.
Automatic tube compensation
This mode is specifically used for weaning and is designed to overcome the resistance of the endotracheal tube by means of continuous calculations. These calculations deal with known resistive coefficients of the artificial airway (size and length), tracheal pressures, and measurement of instantaneous flow.
These calculations allow the ventilator to supply the appropriate pressure needed to overcome this resistance throughout the entire respiratory cycle. To the authors’ knowledge, no studies have proven that this mode is any better than spontaneous breathing trials.
Proportional assist ventilation
This mode was designed to decrease the work of breathing and improve patient-ventilator synchrony. The mode adjusts airway pressure in proportion to the patient’s effort. Unlike other modes in which the physician presets a specific tidal volume or pressure, proportional assist ventilation (PAV) lets the patient determine the inspired volume and the flow rate.
This mode requires continuous measurements of resistance and compliance to determine the amount of pressure to give. The support given is a proportion of the patient’s effort and is normally set at 80%. This support is always changing according to the patient’s effort and lung dynamics.
If the patient’s effort and/or demand are increased, the ventilator support is increased, and vice versa, to always give a set proportion of the breath. The patient’s work of breathing remains constant regardless of his or her changing effort or demand.
This mode can be used only in patients with spontaneous respiratory efforts. PAV has promise, but the US Food and Drug Administration (FDA) has not approved it for commercial use.
Airway pressure–release ventilation
Bilevel, or biphasic, ventilation is a relatively new mode of ventilation that has recently gained popularity. The ventilator is set at 2 pressures (high CPAP, low CPAP), and both levels are time cycled. The high pressure is maintained for most of the time, while the low pressure is maintained for short intervals of usually less than 1 second to allow exhalation and gas exchange to occur.
The patient can breathe spontaneously during high or low pressure (see image below). This mode has the benefit of alveolar recruitment. Its disadvantage is that the tidal volume is variable. The clinician must be constantly aware of the patient’s minute ventilation to prevent severe hypercapnia or hypocapnia.
A Message from Healthsoothe
In an urgent situation or if you get critically ill and are unable to breathe on your own, mechanical ventilation may save your life. It is not intended to cure problems, but it may provide your body with the time it needs to heal.
Some individuals may never be able to breathe unaided again if they have a very acute or deteriorating condition. Regardless of your condition, make sure your physician and family are aware of your medical care preferences.
It is critical to discuss your objectives and establish special instructions and healthcare power of attorney. This might be useful if your loved ones need to make choices on your behalf.
With computer feedback systems, many modern ventilators allow the operator to make fine adjustments in tidal volume, airway pressures, and the timing of the respiratory cycle. The desired result is improved ventilator-patient interaction and limitation of ventilator-induced lung injury.
These newer methods of mechanical ventilation are often based on attractive physiologic hypotheses, and they are interesting to implement.
Each method has its proponents, but objective evidence has failed to show that any of the alternative methods of ventilation is more successful than conventional mechanical ventilation with proper attention to tidal volume. Most clinicians use alternative methods of ventilation only in cases when conventional mechanical ventilation has failed.