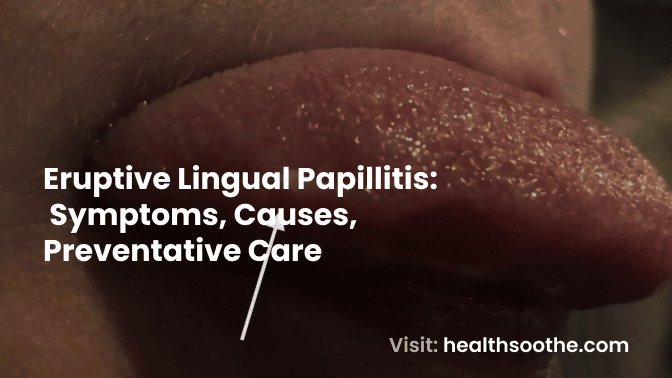
A frequent benign condition known as eruptive lingual papillitis causes the fungiform papillae on the tongue's dorsolateral surface to swell.
- Eruptive lingual papillitis Treatment
- Preventative care for Eruptive lingual papillitis
- Eruptive lingual papillitis symptoms
- Causes of Eruptive lingual papillitis
- What are some protective measures to prevent eruptive lingual papillitis?
- What are the risk factors associated with eruptive lingual papillitis?
- What are the complications of eruptive lingual papillitis?
- Conclusion:
Since 1997, a number of lingual papillitis variations have been documented, most or all of which have painful erythematous papules. Here, we describe a 6-year-old girl who visited the emergency room with a severe variant type of eruptive lingual papillitis that wasn't unpleasant.
Multiple erythematous papules, some of which were white or yellowish in colour, covered the whole dorsal surface of the tongue to a depth of 2-3mm.
The papules were overly swollen, pigmented, clumped together, and crusty. 1Idiopathic in nature, the reason went away after 10 days. Advice to maintain good dental hygiene comforted the parent and patient.
In this unusual case report, lingual papillitis without any past bouts of discomfort is described.
Eruptive lingual papillitis is the name given to an oral rash or inflammation of the papillae.
It is critical to accurately distinguish between acute and chronic papillitis of the tongue and gums. Rashes that are severe can hurt and be uncomfortable.
When it comes to temporary papillitis, its signs typically go away in a few days. The symptoms can be greatly reduced by seeing a dentist.
Eruptive lingual papillitis is an acute stomatitis that typically affects children and has no known cause.
Despite the lack of a definitive cause, scientific literature has suggested that it may be caused by viruses, stress, trauma, food hypersensitivity, and atopic disease.
Because it spreads from one affected person to other family members, 1-3 ELP is also known as eruptive familial lingual papillitis.
Inflammatory swollen blisters (papules), difficulty feeding, and irritability are symptoms of ELP.
Fungiform papillae inflammation is characterised by acute onset, multiple, 2 to 3 mm erythematous papules, and mild to severe pain.
The lingual area's fungiform papillae, which are typically found at the tips, of lateral, and dorsal parts, are included in the papules, which can be red, yellow, or white.
Due to its temporary nature and painful condition, the hypertrophic fungiform papillae have been referred to as transient lingual papillitis (TLP).
Fever, excessive salivation, burning, and adenopathy are the accompanying symptoms. Although lingual papillitis has been discussed in a number of scientific publications, its clinical manifestations still need to be clarified.
This paper presents a case report of a severe variant form of eruptive lingual papillitis that doesn't cause pain. The symptoms disappeared within 10 days and the cause was idiopathic.
This report aims to shed light on a case of non-painful severe variant eruptive lingual papillitis that has never been documented, as well as its diagnosis and treatment.
Read Also: 4 Natural Ways To Boost Your Mood Right Now
Eruptive lingual papillitis Treatment
After 2 or 3 days, the signs of temporary papillitis disappear on their own. But it is important to adhere to certain recommendations in order to avoid eruptive lingual papillitis.
Based on the diagnosis, the doctor will offer specific advice, but the recommended course of action may include: drug treatment.
- Antiviral drugs
- Antibiotics to treat bacterial overgrowth
- Antifungal agents to treat yeast overgrowth.
- Mouthwash medications
- Medications to increase saliva production
- Corticosteroids
Preventative care for Eruptive lingual papillitis
- Diet: Dentists suggest cutting less on hot and acidic meals. Avoid foods that are very spicy; all meals should be medium spicy.
- Using a paste and a brush, brush your teeth at least twice a day.
- It is preferable to clean the oral cavity after eating if the condition is severe.
- treatment of pulpitis, deep caries, and other dental diseases as soon as possible;
- Without entering the stage of complications, treatment of viral and 2inflammatory disorders of the ENT organs and other tissues (tonsillitis, sinusitis, sinusitis; otitis media)
- The body receives enough nutrients, vitamins, minerals, amino acids, trace elements, and other helpful compounds.
- avoiding ingestion of poisonous substances that injure the gums and dental enamel (lemonade, coffee, strong tea)
- kicking harmful behaviours to the curb (alcohol, smoking)
Eruptive lingual papillitis symptoms
The tongue is where papillitis often develops, and many patients compare it to pimples. Even when you aren't eating or drinking, they might still hurt.
Some people report burning, itching, or tingling sensations; in a very small percentage of cases, burning and barely noticeable pain on the tongue. Some people just experience the bump itself as their only sign of discomfort.
Additional symptoms include:
- Eruptive lingual papillitis persist for more than two weeks
- Body temperature rises (fever)
- Soreness of the tongue
- Changes in the tongue colour (in large areas or in the form of dots of white, or red)
If additional severe symptoms appear, the dentist performs additional testing to identify any potentially dangerous conditions.
Only a dentist can diagnose an inflammation by analysing the data from complaints and performing an external and instrumental examination.
Causes of Eruptive lingual papillitis
Eruptive lingual papillitis has an unknown exact cause. Inciting factors have been identified through research:
- Viruses can be causative agents.
- A diet high in sour, spicy, and sweet foods
- Chronic stress
- Chronic trauma to the tongue
- Gastrointestinal complications including constipation
- Allergic reactions
- Improper dental hygiene
- Smoking and frequent alcohol
What are some protective measures to prevent eruptive lingual papillitis?
Simple preventative actions will aid in disease prevention and dental health maintenance. Prevention is preferable to treatment. You needn't wait till you run against this issue.
- Avoid extremely hot meals and beverages, as well as foods and spices that are too salty and spicy. The tongue and the mouth's mucous membranes may have issues as a result.
- Give up chewing or smoking tobacco.
- Don't let any poisons, toxins, or irritants like alcohol (even subpar alcohol), household chemicals, or pesticides get into your mouth.
- Maintaining proper dental hygiene can lessen your risk of contracting an illness that may result in taste bud swelling.
- Avoid biting your tongue or repeatedly rubbing it with your teeth or other things. Be careful when using your toothbrush, avoid over-scrubbing (scrubbing deeply, sometimes with trauma), and avoid rubbing your tongue's surface.
- boosting the immune system and treating severe illnesses that cause red bumps
What are the risk factors associated with eruptive lingual papillitis?
- Smoking and frequent alcohol consumption
- Infections provoked by bacteria, fungi, and viruses
- Allergy
What are the complications of eruptive lingual papillitis?
Eruptive lingual papillitis does not result in any health problems than the usual symptoms. It may result in serious problems if left untreated.
Therefore, timely implementation of diagnostic and therapeutic measures is required. Following the treatment plan exactly as prescribed by the doctor stops the disease from returning.
Conclusion:
This study described the clinical appearance of a 6-year-old girl who had a non-painful severe variant type of eruptive lingual papillitis.
Based on the clinical signs, the ELP condition's lack of pain was rare. Although the diagnosis was made based on the patient's clinical presentation, further research should be done to identify the precise clinical diagnostic standards for ELP.
To clarify an accurate diagnosis, further research must be done on the causes of the symptoms.
Additional resources and citations
- 1Idiopathi
- 2inflammatory disorders
The content is intended to augment, not replace, information provided by your clinician. It is not intended nor implied to be a substitute for professional medical advice. Reading this information does not create or replace a doctor-patient relationship or consultation. If required, please contact your doctor or other health care provider to assist you to interpret any of this information, or in applying the information to your individual needs.