Prior to radiographic alteration, the mineral composition of bone must change by 30–50%. Typically, 10–14 days after histology production is observed, early periosteal new bone may be seen radiographically. There are three types of periosteal reactions: benign, semi-aggressive, and aggressive.
Aggressive responses are not always indicative of [mfn]malignancy[/mfn]; rather, they show that the illness is developing more quickly than the bone can handle it. In general, benign responses are those that are ongoing, homogeneous, and uniform in the thickness and opacity of the bone (solid).
Interrupted responses are often semi-aggressive to aggressive with varied bone opacity and thickness (lamellar, palisading, spiculated, [mfn]amorphous[/mfn]).
Based on activity, periosteal responses should also be specified. In contrast to active reactions, which have hazy, indistinct boundaries, inactive reactions will have defined margins. Finally, the age of the periosteal response may also be used to define it.
While older responses grow thicker and bone-like, younger reactions will be hardly mineralized and opaque like soft tissue. Generally speaking, a periosteal response that is erratic and vague should raise the potential of an aggressive lesion. The periosteal response often does not fit into any of the categories described below.
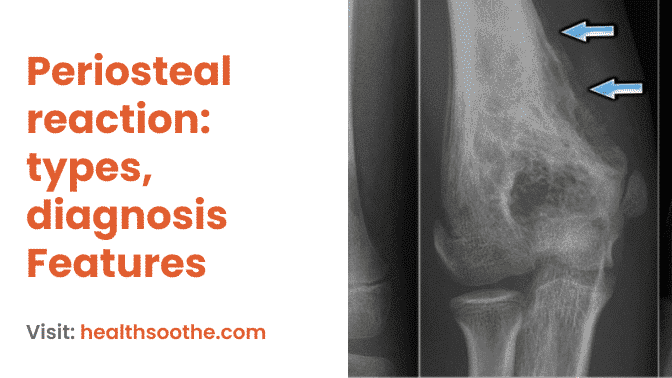
Many aggressive bone lesions exhibit an active periosteal reaction, which is characterised by an irregular rather than a smooth periosteal reaction margin.
There are different levels of periosteal reactivity as well as practically endless different manifestations of an active periosteal reaction.
The periosteal reaction can be detected by the presence of an irregular margin. Because periosteal irregularity is the fundamental change that determines the lesion is aggressive, finding an irregular periosteal margin is more significant than, for example, whether the periosteal reaction is speculated versus columnar.
An aggressive bone lesion is consistent with any indication of periosteal irregularity. A nonaggressive periosteal reaction is distinguished by a smooth edge to the periosteal new bone growth, as one might anticipate.
Because there may be other findings that make the lesion aggressive, the discovery of a smooth periosteal reaction does not necessarily imply that the lesion is not aggressive.
The lesion will still be aggressive if it has a smooth periosteal reaction but an unclear transition zone.
Read Also: Shoe Contact Dermatitis | Causes, Symptoms, Diagnosis
Imagery Differential Diagnosis Features
The periosteal reaction can also be caused by other conditions, but the combination of imaging and clinical findings usually enables accurate diagnosis.
Most of the time, it is easy to distinguish the pattern of symmetric juxtacortical uptake in HOA from the more central and medullary uptake seen in metastatic disease. The spine, pelvis, or ribs are rarely affected by HOA but are frequently affected by metastatic disease.
Hand periosteal reactions can occur with thyroid acropachy, psoriatic arthritis, juvenile rheumatoid arthritis, and human immunodeficiency virus.
However, when limited to the lower extremities, the scintigraphic features should be diagnosed cautiously because lower limb edema or chronic venous stasis may exhibit a similar distribution of uptake.
Types of Periosteal Reaction
Regarding the language used to define periosteal response, there is a significant overlap in the literature.
It has been divided into subtypes that are continuous as opposed to interrupted, single as opposed to numerous layers, and aggressive as opposed to nonaggressive.
Because the disease entities that produce the two main types of periosteal response aggressive and nonaggressive have a large overlap, the main objective in assessing periosteal reaction is to determine its existence rather than the particular subtype.
Radiographically, it is often impossible to tell whether the underlying process is benign or malignant. Aggressive periosteal reactions may result from processes that deposit woven bone quickly over a short period of time, while less intensive processes that advance more slowly give off a nonaggressive look.
- Nonaggressive
- Thin
- Solid
- Thick irregular
- Septated
- Aggressive
- Laminated (onionskin)
- Spiculated
- Perpendicular/hair-on-end
- Sunburst
- Disorganized
- Codman triangle
Even if there is a great deal of overlap, the subtype of periosteal response sometimes points to a particular illness. For instance, the nonaggressive type of solid periosteal response is most often associated with gradual, benign processes. The solid periosteal response may manifest as thin or thick sheets in osteomyelitis, osteoid osteoma, and healed fractures.
A laminated or onionskin-like look is created when several layers of new bone grow concentrically around the cortex in the laminated subtype of periosteal response. Concentric layers were once thought to emerge as a result of alternating cycles of fast and gradual damage to the bone.
More recent research, however, contends that the multiple layers develop as a result of fibroblast sheets in the nearby soft tissue being modulated; these sheets then acquire osteoblastic potential and give rise to sheets of new bone.
Another theory is that the inner cambium layer is stimulated to form a new bone layer below as the new layer of bone is lifted off the cortex. Numerous lesions, including sarcomas, osteomyelitis, and chondroblastomas, have a laminated appearance.
How long does a periosteal reaction take?
5 days after the fracture, the periosteal reaction was first noted and was found in 62% of the films taken between 15 and 35 days later. Soft callus first appeared on day 12 and was common in 41% of cases between days 22 and 35.
At day 19, hard callus and bridging started to appear, and their prevalence increased to 60% after 36 days.
Numerous conditions and injuries can lead to periosteal reactions, including fracture healing, chronic stress injuries, subperiosteal hematomas, osteomyelitis, and bone cancer. These conditions include hypertrophic osteopathy, chronic stress injuries, and subperiosteal hematomas. It might also manifest as a severe symptom of Graves’ disease, an autoimmune thyroid illness, known as thyroid acropachy.
Menkes kinky hair syndrome and hypervitaminosis are additional causes.
It can take three weeks for it to materialise.
Conclusion:
Cortical bone reacts to various insults by forming a periosteal reaction. The most crucial stage is the identification of the periosteal reaction.
The periosteal reaction pattern can occasionally be very suggestive of a specific process, but generally speaking, the disease entities that lead to aggressive and nonaggressive forms share a lot of similarities.
periosteal reactions typically result from intense, fast-acting processes, whereas nonaggressive reactions typically come from slower, indolent processes. The periosteal reactions can be caused by a variety of things, including trauma, infection, arthritis, tumours, drug use, and vascular entities. When periosteal reaction manifests bilaterally, a systemic disease process should be taken into account.