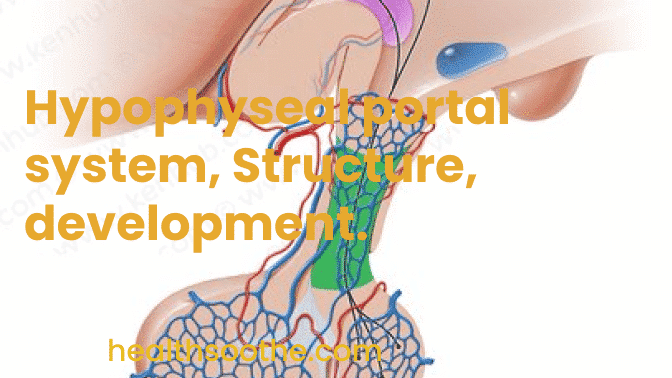
The hypophyseal portal system is a network of blood arteries that connects the anterior pituitary and hypothalamus at the base of the brain.
Its principal job is to swiftly transfer and exchange hormones between the anterior pituitary gland and the hypothalamic arcuate nucleus.
The portal system's capillaries are fenestrated (have many tiny channels with high vascular permeability), enabling quick communication between the hypothalamus and pituitary.
Gonadotropin-releasing hormone, corticotropin-releasing hormone, growth hormone-releasing hormone, and thyrotropin-releasing hormone are among the principal hormones that the system transports.
The hypophyseal portal system is a network of blood arteries that connects the anterior pituitary and hypothalamus at the base of the brain.
Through a hypothalamic hypophyseal portal system, [mfn]hypothalamic hormones[/mfn] that release or block anterior pituitary hormones go to the anterior pituitary. Normal blood flow involves the heart pumping blood via an artery, a capillary, a vein, and then back to the heart.
A portal system is one in which blood travels from one capillary network into a portal vein, then into a second capillary network, before returning to the heart. The second capillary network's location is indicated by the name of the portal system. Blood travels through portal veins in the hypophyseal portal system from capillaries in the hypothalamus to capillaries in the anterior pituitary.
In other words, the hormones that are transported by the hypothalamohypophyseal portal system enable communication between the anterior pituitary and hypothalamus and create a crucial link between the nervous and endocrine systems.
Blood enters the hypothalamus through the superior hypophyseal arteries, which branch off of the medial internal carotid artery just after leaving the cavernous sinus. The primary capillary network in the median eminence is formed by the superior hypophyseal arteries, which first appear 5 mm distal to the origin of the ophthalmic artery.
These arteries split into a capillary network known as the primary plexus of the hypophyseal portal system at the intersection of the infundibulum and the median eminence of the hypothalamus. The pars distalis receives blood from this capillary plexus.
Blood exits the primary plexus and travels down the outside of the infundibulum into the anterior and posterior hypophyseal portal veins. Peptides that are released at the median eminence enter the primary plexus using this system.
From there, the peptides would travel through the hypophyseal portal veins and the secondary plexus to reach the adenohypophysis.
The pituitary and hypothalamus could communicate with one another thanks to the fenestrated capillaries in the portal system. The anterior pituitary releases hormones when peptides bind to G-protein-coupled receptors that are expressed in the cells of the adenohypophysis.
The secondary plexus of the hypophyseal portal system is a capillary network formed in the anterior pituitary by the division of the hypophyseal portal veins once more. Blood is removed from the anterior pituitary by hypophyseal veins.
The pituitary gland's primary and secondary capillary plexuses, along with any connecting hypophyseal portal veins, make up the hypophyseal portal system.
Read Also: Mandibular Hypoplasia: Causes, Symptoms, Treatment, And Surgery
Structure of Hypophyseal portal system
Injection and vascular corrosion casting techniques have been used for many years on laboratory animals and human cadaver specimens to study the blood supply and flow direction in the hypophyseal portal system.
The neural and anterior pituitary lobes are connected by short portal vessels, which allow for quick hormonal exchange.
Anatomical evidence for confluent interlope vessels specifically within and between the pituitary lobes includes venules supplying blood from the anterior to the neural lobe and capillary shunts transferring blood between the intermediate and neural lobes.
These microvascular structures suggest that the pituitary gland's lobes exchange information on-the-fly.
Other research findings demonstrated that the superior hypophyseal arterial system's ascending and descending infundibular branches and capillaries provide arterial blood to the neural hypophyseal stalk and the ventromedial area of the hypothalamus arcuate nucleus.
Blood is also supplied to hypophyseal arteries by tiny ascending vessels that emerge from the anastomoses that join the upper and lower hypophyseal artery systems.
A lot of these branches are continuous between the anterior pituitary and the proximal arcuate nucleus, allowing for quick hormone exchange.
According to further data, the median eminence and arcuate nucleus' capillary perivascular spaces are connected, which may help the ventral hypothalamus receive hormonal signals from the systemic circulation.
Hypophyseal portal system Development
Other research findings demonstrated that the superior hypophyseal arterial system's ascending and descending infundibular branches and capillaries provide arterial blood to the neural hypophyseal stalk and the ventromedial area of the hypothalamus arcuate nucleus.
Blood is also supplied to hypophyseal arteries by tiny ascending vessels that emerge from the anastomoses that join the upper and lower hypophyseal artery systems.
A lot of these branches are continuous between the anterior pituitary and the proximal arcuate nucleus, allowing for quick hormone exchange.
According to further data, the median eminence and arcuate nucleus' capillary perivascular spaces are connected, which may help the ventral hypothalamus receive hormonal signals from the systemic circulation.
Control of anterior pituitary secretion regulation of anterior pituitary secretion by the hypothalamus occurs as follows:
- Neurosecretory cells are clumps of neurons that are located above the optic chiasm. They produce the hormones that release and suppress the hypothalamus in their cell bodies. The hormones are then packaged into vesicles and transported quickly down axons to the axon terminals, where they are stored.
- Nerve impulses cause the vesicles to exocytose when the hypothalamus' neurosecretory cells are excited. The primary plexus of the hypophyseal portal system then receives the hypothalamic hormones, which then diffuse into the blood.
- The blood swiftly carries the hypothalamic hormones into the secondary plexus via the hypophyseal portal veins. Through this direct pathway, hypothalamic hormones can reach anterior pituitary cells without being diluted or destroyed by the general circulation. The anterior pituitary cells and hypothalamic hormones interact within the secondary plexus, where the hormones diffuse from the bloodstream. The anterior pituitary cells produce hormones that are secreted into the secondary plexus capillaries in response to stimulation by the appropriate hypothalamic-releasing hormones.
- The anterior pituitary hormones exit the secondary plexus capillaries and enter the hypophyseal veins, where they are released into the bloodstream. The body's target tissues are then reached by anterior pituitary hormones. Tropins are the name for the anterior pituitary hormones that affect other endocrine glands.
Conclusion:
The hypothalamus has two mechanisms for controlling growth hormone release. Growth hormone-releasing hormone (GHRH) stimulates growth hormone release; somatostatin, a different hormone peptide sometimes known as growth hormone-inhibiting hormone (GHIH), suppresses it.
IGF-1, an insulin-like growth factor, offers counterproductive feedback by preventing somatotrophs from releasing growth hormones. In somatotrophs, thyroid hormones (T3 and T4) promote the production of the growth hormone gene.