A needle is inserted into the pleural space surrounding your lungs during a minimally invasive procedure called a thoracentesis. To make it simpler for you to breathe, the intention is to drain fluid or air.
A pleural tap or thoracentesis is a procedure used to drain extra fluid or air from your pleural space.
The tiny space between your lungs and chest wall is known as the pleural space. Pleural effusion refers to an accumulation of fluid in your pleural space. Your lungs may become compressed by pleural effusion, making breathing difficult.
In order to differentiate between exudate, which may be caused by inflammatory or cancerous conditions, and transudate, which may be caused by the failure of organ systems that affect fluid balance in the body, a thoracentesis is used as a diagnostic procedure. This analysis assists in identifying the abnormality's root cause.
Some conditions that can cause pleural effusion to include:
- Cancerous tumours
- Pneumonia or other lung infections
- Congestive heart failure
- Liver failure is known as cirrhosis
What is a thoracentesis?
A needle is inserted into the pleural area around your lungs during a minimally invasive technique called a thoracentesis.
To make it simpler for you to breathe, the aim is to drain fluid or air. In some circumstances, the procedure will also assist your doctor in identifying the origin of your fluid accumulation.
Depending on the underlying disease you have, your doctor may drain more or less fluid. The National Institute of Heart, Lung, and Blood
According to Trusted Source, the procedure usually takes 10 to 15 minutes, although it can take longer if your pleural area is filled with a lot of fluid. To determine the reason for fluid buildup around one or both of your lungs, a pleural fluid analysis, and a lab test, may be carried out after thoracentesis.
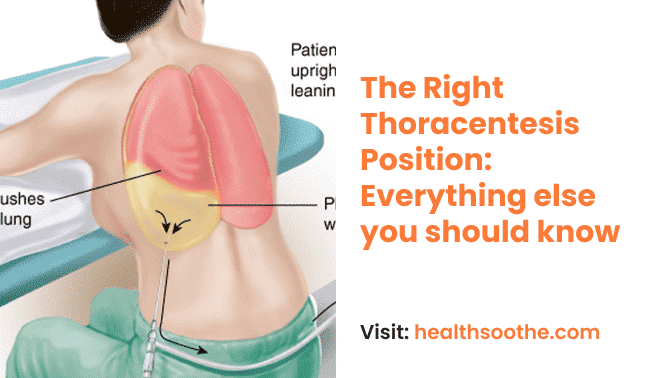
Thoracentesis Position
You'll be lying on a hospital bed in a sitting posture. You'll be leaning your arms against the bedside table.
This posture aids in spreading out the needle's entry points between the ribs. You can lie on your side on the edge of the bed if you are unable to sit.
Note:
The thoracentesis location should be one to two intercostal spaces below the maximum level of the effusion, in the mid-scapular or posterior axillary line, 6 to 10 cm lateral to the spine.
A pleural biopsy may also be carried out by your doctor. It may aid in determining the underlying cause of pleural effusion despite not being routinely done. Possible reasons include:
- The presence of cancer cells, such as lung cancer
- Mesothelioma1https://www.nhs.uk/conditions/mesothelioma/#:~:text=Mesothelioma%20is%20a%20type%20of,usually%20linked%20to%20asbestos%20exposure. is an asbestos-related cancer of the tissues that cover your lungs
- Pleural tuberculosis
What is the procedure for a thoracentesis?
- Either a hospital or a doctor's office may do a thoracentesis. Although it's usually done with you awake, you could be given a sedative. If you've been given sedation, you'll want assistance getting home following the treatment.
- You'll be placed in a position that enables your doctor to reach your pleural area after sitting in a chair or reclining on a table.
- Your doctor should use an ultrasound to make sure the needle will go into the right spot. They may sometimes additionally employ CT guidance.
- After cleaning, a numbing chemical will be administered to the chosen location.
- Between your ribs, your doctor will place the needle or tube to access your pleural region. Throughout this procedure, you could feel an unpleasant pressure, but try to remain completely still. After then, the extra liquid will be emptied off.
- A bandage will be applied to the insertion site when all the fluid has been removed.
- Right after the thoracentesis, your doctor could take a follow-up X-ray.
- They could ask you to spend the night in the hospital or clinic so you can be observed, depending on the severity of your symptoms and to make sure there are no problems.
Who might need a thoracentesis
Patients with pleural effusion undergo a thoracentesis to either help them breathe easier or to help with a diagnosis.
According to the American Thoracic Society, the following are the most frequent justifications for thoracentesis:
- To diagnose the cause of the new pleural effusion
- To improve comfort
- To diagnose cancer or improve cancer symptoms
- To diagnose a suspected infection
If you're a good candidate for thoracentesis, your doctor can decide.
Thoracentesis may not be possible for certain individuals. If you don't have enough pleural fluid, or if you have an infection or incision where the needle will be inserted, you may not be a suitable candidate for thoracentesis.
Additionally, doctors are hesitant to conduct thoracentesis on patients who:
- Can’t be safely repositioned
- Have bleeding disorders
- Are taking blood thinners
- May have scarring from recent lung surgery
- Have other conditions where potential complications outweigh benefits
How to Prepare for a thoracentesis
A thoracentesis requires no particular preparation. However, if you have any queries or worries regarding the operation, talk to your doctor. Tell your doctor if you also:
- Are currently taking medications, including blood thinners like aspirin, clopidogrel (Plavix), or warfarin (Coumadin)
- Are allergic to any medications
- Have any bleeding problems
- May be pregnant
- Have lung scarring from previous procedures
- Currently, have any lung diseases like asthma or emphysema
Some risks that come with the procedure
There are dangers associated with any invasive surgery, although thoracentesis seldom causes adverse effects. Potential dangers include:
- Pain
- Bleeding
- Bruising
- Air accumulation (pneumothorax) pushes on the lung, causing a collapsed lung
- Infection
Conclusion:
A thoracentesis is a minimally invasive technique in which a doctor uses a needle to extract air or fluid from the pleural area around your lungs. It is often carried out to aid in the diagnosis or to enhance breathing.
Slight issues like bleeding at the injection site or minor bruises are the most frequent thoracentesis consequences. Some patients have more serious side effects including liver or spleen damage.
Your doctor can explain the possible dangers and advantages of thoracentesis to you and help you decide whether you're a suitable candidate.
Additional resources and citations
- 1https://www.nhs.uk/conditions/mesothelioma/#:~:text=Mesothelioma%20is%20a%20type%20of,usually%20linked%20to%20asbestos%20exposure.
The content is intended to augment, not replace, information provided by your clinician. It is not intended nor implied to be a substitute for professional medical advice. Reading this information does not create or replace a doctor-patient relationship or consultation. If required, please contact your doctor or other health care provider to assist you to interpret any of this information, or in applying the information to your individual needs.