Share this post
Most times, traumatic brain injuries lead to certain morbid brain conditions that compromise how the organs of the body function, and this is why it is very crucial to treat abnormal brain conditions with immediate effect before it leads to dirge side effects including death.
Today, we will expatiate on one of such brain conditions commonly known as midline brain shift, which is also known as midline shift or brain shift.
This article will explain what this midline brain shift looks like, its causes, its treatments, and how it can be prevented.
We move!
Midline Brain Shift – What is this Brain Shift or Midline Shift All About?
Midline brain shift refers to a shift (displacement) of brain tissue across the centerline of the brain.
It may occur following traumatic brain injury in association with raised intracranial pressure or an intracranial hematoma which can push the brain towards one side causing a midline shift.
Midline brain shifts cause extreme pressure on parts of the brain resulting in the blood supply to various parts of the brain being compromised. This can be fatal and is considered a medical emergency.
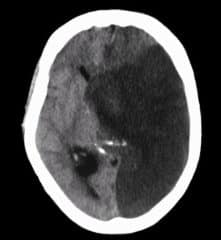
Midline brain shift may be evident in neuroimaging such as CT scanning. The sign is considered ominous because it is commonly associated with a distortion of the brain stem that can cause serious dysfunction evidenced by abnormal posturing and failure of the pupils to constrict in response to light.
Watch the video below to learn more:
Symptoms of Midline Brain Shift
Midline shift is often associated with high intracranial pressure (ICP), which can be deadly. In fact, midline shift is a measure of ICP; the presence of the former is an indication of the latter.[mfn]https://en.wikipedia.org/wiki/Midline_shift[/mfn] The presence of midline shifts is an indication for neurosurgeons to take measures to monitor and control ICP.
The main causes of elevated intracranial hypertension symptoms are papilledema and neurological irritation, compression, or displacement. Almost all cases of non-specific headaches are recorded, and they are probably mediated by the trigeminal nerve's pain fibers in the dura and the brain's blood vessels.
Pain is typically diffuse and worse in the mornings, and the Valsalva maneuver can exacerbate it. Vomiting and nausea are frequent symptoms of high intracranial pressure. Patients who have CN VI palsy from compression and horizontal diplopia are more likely to present with double vision.
Frequent transient visual abnormalities can cause one or both eyes to gradually lose vision, which is how they are frequently described. The worsening of visual anomalies is caused by posture changes.
It is possible to report peripheral vision loss, which typically starts in the nasal inferior quadrant and progresses to loss of the central visual field. Visual acuity changes that include blurring or distortion could happen.
There may be varying degrees of color distinction loss. Intraocular hemorrhage can cause a sudden loss of vision in more severe or chronic cases. It is possible to experience pulsing tinnitus that is made worse by supine or bending positions and the Valsalva maneuver.
Radicular pain, numbness, or paresthesias are potential symptoms that are frequently linked to localized compression of the brain or potential brain herniation. Neurological findings can indicate a serious illness.
The subfalcine, central transtentorial, uncal transtentorial, cerebellar tonsillar/foramen magnum, and transcalvarial lobes are the anatomical regions where the herniation is most likely to happen.
Consciousness or responsiveness may decline as a result of these kinds of changes. Depending on whatever part of the brain has herniated, specific neurological constellations may exist.
Due to the local impact of mass lesions or pressure on the reticular formations of the midbrain, this often ends in a stupor state or more seriously in a coma. It could also result in respiratory impairment.
Other signs of midline brain shift include the following:
- Difficulty maintaining balance.
- A constant sense of imbalance.
- Inappropriate posture.
- Efficient weight distribution on the balls of the feet.
- Abnormal gait or walk.
- Changes in the sense of direction.
- “Odd” perceptions of one's position in space

Causes of Midline Shift Brain
Midline brain shift can be caused by conditions including traumatic brain injury, stroke, hematoma, or birth deformity that leads to a raised intracranial pressure.
Methods of Detection of Midline Brain Shift
Doctors detect midline shifts using a variety of methods. The most prominent measurement is done by a computed tomography (CT) scan and the CT Gold Standard is the standardized operating procedure for detecting MLS.
Since the midline shift is often easily visible with a CT scan, the high precision of Magnetic Resonance Imaging (MRI) is not necessary, but can be used with equally adequate results.
Newer methods such as bedside sonography can be used with neurocritical patients who cannot undergo some scans due to their dependence on ventilators or other care apparatuses. Sonography has proven satisfactory in the measurement of MLS but is not expected to replace CT or MRI.
Automated measurement algorithms are used for exact recognition and precision in measurements from an initial CT scan. A major benefit to using automated recognition tools includes being able to measure even the most deformed brains because the method doesn’t depend on normal brain symmetry.
Also, it lessens the chance of human error by detecting MLS from an entire image set compared to selecting the single most important slice, which allows the computer to do the work that was once manually done.
Structures Associated with the Midline Brain Shift
Three main structures are commonly investigated when measuring midline shifts. The most important of these is the septum pellucidum, which is a thin and linear layer of tissue located between the right and left ventricles. It is easily found on CT or MRI images due to its unique hypodensity.
The other two important structures of the midline include the third ventricle and the pineal gland, which are both centrally located and caudal to the septum pellucidum.[mfn]https://www.verywellhealth.com/the-brain-can-undergo-a-midline-shift-1720044[/mfn]
Identifying the location of these structures on a damaged brain compared to an unaffected brain is another way of categorizing the severity of the midline shift. The terms mild, moderate, and severe are associated with the extent of increasing damage.
Diagnosing the Midline Brain Shift
Midline shift measurements and imaging has multiple applications. The severity of brain damage is determined by the magnitude of the change in symmetry. Another use is secondary screening to determine deviations in brain trauma at different times after a traumatic injury as well as initial shifts immediately after.
The severity of shift is directly proportional to the likeliness of surgery having to be performed. The degree of MLS can also be used to diagnose the pathology that caused it.
The MLS measurement can be used to successfully distinguish between a variety of intracranial conditions including acute subdural hematoma, malignant middle cerebral artery infarction, epidural hematoma, subarachnoid hemorrhage, chronic subdural hematoma, infarction, intraventricular hemorrhage, a combination of these symptoms, or the absence of pertinent damage altogether.
Treatments of Midline Shift Brain
Immediate surgery may be indicated when there is a midline shift of over 5 mm. The most important treatment when a midline shift is present is relieving the pressure that is pushing the brain off-center.
If a collection of blood is the cause, such as a subdural hematoma, surgery will be needed to remove the blood clot and stop the bleeding. Antibiotics are used to treat infection and steroids may be used to decrease inflammation and swelling.
An intensive care unit (ICU) environment requires constant monitoring in the event of a rapid rise in intracranial pressure, which is a neurosurgical emergency.
A patient with acute intracranial hypertension should initially be stabilized, with medical personnel working for hemodynamic stability and avoiding and addressing any aggravating or precipitating causes.
These patients need to have their heart rate, blood pressure, body temperature, oxygenation, ventilation, blood glucose, input, and ECG closely monitored. Monitoring of intracranial pressure should also be performed in patients with suspected intracranial hypertension, particularly those with severe traumatic brain injury.
It is crucial to avoid and address conditions that could worsen or trigger intracranial hypertension. The following measures are taken to buy time until the underlying cause is found and fixed:
- To reduce venous outflow resistance and enhance cerebral spinal fluid displacement from the intracranial to the spinal compartment, keep the head neutrally positioned and elevated to 30 degrees.
- Intracranial pressure may rise in both hypoxia and hypercapnia. It is essential to manage your breathing properly to keep your intracranial pressure under control. To maintain a normal PaCO2 and sufficient oxygenation without raising the PEEP, ventilation control is crucial.
- Blood pressure and intracranial pressure can both rise as a result of agitation and pain. An essential adjunctive treatment is providing adequate analgesia and sedation. Medication with a negligible hypotensive effect should be preferred because the majority of sedatives can affect blood pressure.
- Before giving out sedatives, hypovolemia should be treated because it can hasten the hypotensive side effects. The advantage of shorter-acting drugs is that sedation can be briefly interrupted to assess neurological status.
- Fever can speed up the metabolism of the brain and is a powerful vasodilator, both of which increase cerebral blood flow and intracranial pressure. Antipyretics and cooling blankets should be used to reduce fever, and infectious causes must be ruled out.
Complications of Midline Shift Brain
Midline brain shift causes extreme pressure on parts of the brain resulting in the blood supply to various parts of the brain being compromised. This can be fatal and is considered a medical emergency.
Is Midline Brain Shift Dangerous?
Midline shift brain is considered ominous because it is commonly associated with a distortion of the brain stem that can cause serious dysfunction evidenced by abnormal posturing and failure of the pupils to constrict in response to light.
Final Words
Depending on the source, midline shift symptoms might range from benign to fatal. Children often have a longer tolerance for increased intracranial pressure (ICP).
The brain is naturally balanced between the left and the right hemispheres. On a computed tomography (CT) scan that looks down at the brain from the top of the head, there is a groove that runs between both sides of the brain that is midline to the body.
The spinal cord emerges at the middle base of the brain and continues down the center of the back. A midline shift occurs when something pushes this natural centerline of the brain to the right or to the left. It is a concerning sign after head trauma.
A number of studies have examined the effects of midline shifts on long-term outcomes. Since a midline shift happens due to bleeding and pressure, the amount of bleeding, the location of damage, and the overall level of pressure experienced by the brain are all important considerations.
When the brain moves, this causes trauma to other structures as they are pulled and pushed out of their natural position. The greater the midline shift, the more serious the complications and the greater the risk of death.

I Am odudu abasi a top-notch and experienced freelance writer, virtual assistant, graphics designer and a computer techie who is adept in content writing, copywriting, article writing, academic writing, journal writing, blog posts, seminar presentations, SEO contents, proofreading, plagiarism/AI checking, editing webpage contents/write-ups and WordPress management.
My work mantra is: “I can, and I will”