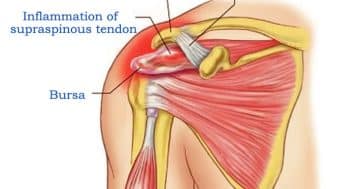
The supraspinatus muscle is located in the supraspinatus fossa behind the scapula. It is connected to the supraspinatus tendon – a thick fibrous band of tissue that connects the supraspinatus muscle to the shoulder joint.
[ninja_tables id=”73347″]
The supraspinatus tendon is a part of the rotator cuff. The function of the supraspinatus is to facilitate the movement of the arm upwards. When there is damage or injury to the supraspinatus tendon, it is referred to as supraspinatus tendinosis, which is also known as supraspinatus tendinopathy.
The average age of onset of this complication is in one’s 50s due to degeneration during the normal process of aging when all of the tendons of the rotator cuff start to become weak as the muscle becomes weaker. Diabetic patients are more prone to the condition.
It is also a common cause of shoulder pain in athletes whose sports involve throwing and overhead motions (tennis or badminton as it involves raising the arms frequently and repetitively above shoulder level).
Today’s article will explain all there is to know about supraspinatus tendinosis; its symptoms, causes, treatments, and what you can do to prevent it from happening to you.
Let’s proceed.
The Overview of Supraspinatus tendinosis
Supraspinatus tendinosis, also known as supraspinatus tendinopathy is a common and crippling condition that becomes more prevalent after middle age[mfn]https://www.physio-pedia.com/Supraspinatus_Tendinopathy[/mfn]. It is a common cause of shoulder pain.
The supraspinatus tendon lies in the subacromial space and is a part of the rotator cuff muscles. Overuse of the supraspinatus tendon is attributed to be the principal factor that predisposes to this condition.
The Supraspinatus tendon of the rotator cuff becomes degenerated most often as a result of repetitive stresses and overloading during sports or occupational activities, paving the way for tendinopathy. The tendon of the supraspinatus commonly impinges under the acromion as it passes between the acromion and the humeral head.
Watch the video below for more info on what supraspinatus tendinosis is all about:
Symptoms and Causes of Supraspinatus Tendinosis
As stated above, overuse is the principal cause that leads to supraspinatus tendinopathy, and also tendon impingement[mfn]https://en.wikipedia.org/wiki/Shoulder_impingement_syndrome[/mfn] is one of the main causes of supraspinatus tendinopathy, which could be due to subacromial loading. Other causes include rotator cuff overload and muscle imbalance.
People affected with the condition may have progressive subdeltoid aching and it gets worse by abduction, elevation, or sustained overhead activity.
There may be tenderness and a burning sensation around the shoulder as well. Pain is felt in the arm and behind the shoulder while moving the arm upwards like waving at someone. The pain may radiate to the lateral upper arm or may be located in the top and front of the shoulder.
Activities over the head typically make the pain worse. In the beginning, pain is felt only during activities, but at the later stages even at rest, pain can be experienced.
It could be an underlying supraspinatus tendinosis if the person affected indicates the following:
- Pain increases with reaching
- Pain is felt after frequent repetitive activity at or above the shoulder
- The patient feels weakness in resisted abduction and forward flexion, especially with pushing and overhead movements
- The patient has difficulty sleeping at night due to pain, especially when lying on the affected shoulder, and with an inability to sleep
- The patient has difficulties with simple movements, such as brushing hair, putting on a shirt or jacket or reaching the arm above shoulder height
- The patient has a limited range of motion in the shoulder
- The patient had a former shoulder trauma
The shoulder may be warm to the touch and there may be fullness anterolaterally. Furthermore, the arc of motion can generate pain between 70° and 120° of abduction.
Anterior instability leading to posterior tightness is generally associated with supraspinatus tendinosis. The person may complain of pain, inflammation, decreased range of motion, strength, and functional activity.
Differential Diagnosis of Supraspinatus Tendinosis
In general, the causes of an acute painful shoulder can be classified into different categories, according to the prevailing patho-anatomy. These include:
- Acromioclavicular Joint Injury
- Bicipital Tendinopathy
- Brachial Plexus Injury
- Cervical Disc Injuries
- Cervical Discogenic Pain Syndrome
- Cervical Radiculopathy
- Cervical Spine Sprain/Strain Injuries
- Clavicular Injuries
- Contusions
- Degenerative causes like rotator cuff tear, cervical spine radiculopathy, and osteoarthritic glenohumeral joint
- Infraspinatus Syndrome
- Infective causes like acute pyogenic arthritis and osteomyelitis
- Inflammatory causes like gouty arthritis, adhesive capsulitis or frozen shoulder and calcific tendinopathy
- Myofascial Pain in Athletes
- Neoplastic causes like tumor metastasis
- Shoulder Dislocation
- Subacromial impingement
- Superior Labrum Lesions
- Swimmer’s Shoulder
- Traumatic fractures and dislocations
More probing investigations can narrow down the differential diagnoses, which could include: blood for white cell counts, search for abnormal blood biochemistry and inflammatory markers, as well as radionuclide imaging and MRI.
Outcome Measures
Diagnosis is usually clinical, but imaging can be useful. Shoulder x-rays can reveal calcifications in the rotator cuff tendons and in the bursa. In long-standing cases, there may be degenerative changes, such as cystic/sclerotic changes at the greater tuberosity and decreased humeral head-acromion distance, secondary to upward migration of the humeral head.
In acute calcific tendinopathy, calcifications may be irregular, fluffy, and ill-defined. Dynamic ultrasound can demonstrate thickening of the subacromial bursa and impingement during an abduction. Magnetic resonance imaging (MRI), rather than computed tomography (CT), is the preferred modality since it produces more detailed soft-tissue images.
Examination
The anamnesis often reveals that, in case of a calcification, due to trauma, pain emerges later on, after a few hours.
The physical examination consists of taking the fever, looking for external wounds or bruises over the affected shoulder, and checking the skin temperature. Further, the examiner will palpate the area of the tendinous insertion of the supraspinatus muscle for checking tenderness and pain. Both passive and active movements will be performed.
Specific questionnaires can be used like; the Simple Shoulder Test (SST) and Oxford Shoulder Score (OSS).
With clinical examination, other causes of shoulder pain should be excluded. So, the neck, shoulder, and chest wall have to be examined.
The shoulders are inspected for symmetry, localized swelling, and muscle atrophy. There may be tenderness below the acromion and over the greater tuberosity. Internal rotation of the shoulder can facilitate palpation of the supraspinatus insertion on the greater tuberosity.
The most important clinical maneuvers are as follows:
- Painful arc
Testings:
- Neer’s sign
- Hawkin’s sign
- Supraspinatus challenge test = “The Empty Can” sign = Job‘s test
- Drop arm test
- Impingement test
If sonography is done, the standard method for sonographic evaluation of the supraspinatus tendon requires the arm behind the back (Crass position) or hand on the back pocket (modified Crass position).
Yet diagnosis is usually clinical, but imaging can be useful. Shoulder x-rays can reveal calcifications in the rotator cuff tendons and in the bursa. In long-standing cases, there may be degenerative changes, such as cystic/sclerotic changes at the greater tuberosity and decreased humeral head-acromion distance, secondary to upward migration of the humeral head.
In acute calcific tendinosis, calcifications may be irregular, fluffy, and ill-defined[mfn]Supraspinatus Tendonitis – StatPearls – NCBI Bookshelf – NIH[/mfn]. Dynamic ultrasound can demonstrate thickening of the subacromial bursa and impingement during an abduction. Also, sonography and Magnetic resonance imaging (MRI) can be done.
Supraspinatus tendinosis can be graded using a modified 4-point scale from 0 to 3 based on previous studies. Diagnosis is based on the appearance of the rotator cuff tendons (grading system) and the presence or absence of signs denoting involvement of the subacromial bursa and subacromial–subdeltoid plane
Treatment and Medical Management of Supraspinatus Tendinosis
Conservative approach is the first line of treatment for the condition by avoiding activities that may aggravate the condition and applying heat and cold, and doing stretching exercises.
Treatment begins with measures to relieve pain and inflammation by prescribing pain medications and NSAIDs. This will bring down the pain and inflammation. The next mode of treatment is to strengthen the muscles and tendons that form a part of the supraspinatus.
The person affected with the condition cannot move the arm as easily as he/she used to because of the weakness of the tendons. In order to overcome this, the physiotherapist will formulate strengthening exercises.
Exercises that increase the range of the shoulder will also be designed by the physiotherapist as the motion of the shoulder is affected severely by this condition.
Therapeutic exercises are found to be effective for remodeling and strengthening degenerated tendons in the supraspinatus. Bracing is another form of passive modality treatment for supraspinatus tendinopathy
Once the strength starts to return and the arm can be moved without much difficulty, a gradual return to activities of daily living is recommended. As for the complete recovery and healing of the condition, it may take anywhere between a couple of weeks to four weeks, till then complete return to normal activities is not advised.
However, if you are a person who takes part in sports or your job involves rigorous overhead activities, it may take two weeks.
It should be understood that tendinopathies are a highly prevalent problem in the musculoskeletal specialty of medicine and the doctor will prescribe the correct treatment modality after a thorough physical examination and medical tests, if necessary.
The treatment used to manage supraspinatus tendinosis depends on the etiology of the pathology. At first, conservative treatment is preferred. This treatment involves physical therapy, nonsteroidal anti-inflammatory drugs (NSAIDs), ice treatments, and resting.
Corticoid injections can also be used in addition to physical therapy. Surgical intervention can be a solution if there is no improvement after 3-6 months of conservative treatment.
NSAIDs may be the first choice for mild to moderate symptoms if there are no contraindications to these agents. A short-term use (7-14 days) of NSAIDs is useful to relieve the pain associated with tendinitis. However, there is little evidence supporting a long-term course of NSAIDs.
Moderate to severe symptoms may require a local subacromial corticosteroid injection. The major indications for surgery are ongoing pain, loss of function, failure to respond to conservative therapy for 3 months, or evidence of an acute tear in a younger patient.
Surgical approaches include calcium deposit resection, with or without subacromial decompression, bursal resection, and acromioplasty, using either arthroscopic or open methods. It’s also possible to split off the coracoacromial ligament to enlarge the space between the acromion and humerus.
This can cause instability, but we can compensate for it with some training of the rotator cuff. With physical therapy, it takes patients up to 4 months to recover. The goal of surgery is to obtain pain relief, increased range of motion, and increased power.
Bursal resection: Removement of the subacromial bursa.
Acromioplasty: Generally, it implies the removal of a small piece of the surface of the acromion that is in contact with a tendon causing, by friction, damage to the latter tissue.
Physical Therapy Management
The main goal in the acute phase (initial phase) is to alleviate pain and inflammation, prevent aggravation of pain, reduce muscle wasting and normalize the arthrokinematics of the shoulder girdle. A period of rest should be considered in order to avoid further aggravation and shoulder discomfort.
Passive modalities should be considered in order to avoid painful aggravation. Modalities such as ultrasound, cryotherapy, and electrical muscle stimulation can provide temporary relief in the acute phase.
Strengthening exercises such as isometric exercises should be considered in order to work out the shoulder girdle musculature. Proper home exercise programs should also be taught in conjunction with proper ergonomics.
The management of supraspinatus tendinosis consists of different progressive exercises. There are three phases of treatment: Immobilization, passive/assisted range of motion, and progressive resistance exercises.
Early management includes avoidance of repetitive movements that aggravate the pain. Patients should be informed about pain-provoking postures and movements. Cryotherapy, soft tissue techniques, and wearing a sling/taping are some other techniques to relieve pain.
Gentle range-of-motion exercises, such as Codman’s classic pendulum exercises, maintain range of motion and prevent the development of adhesive capsulitis. Once the pain has been reduced, joint mobilizations, massages, muscle stretches, and active exercises are needed to improve the ROM again.
Active-assisted mobilizations can be done by the patient himself/herself by using an exercise bar. We can also use a rope and pulley, this way the unaffected arm is able to pull the affected one into anteversion.
Strengthening exercises should work on the external rotators, internal rotators, biceps, deltoid, and scapular stabilizers. Strengthening these muscles will keep the shoulder joint more stable and prevent further injuries. Eccentric exercises will also be more effective than concentric exercises.
I.E.:
- Side-lying external rotation with a dumbbell against gravity
- Prone horizontal abduction with a dumbbell against gravity
- Prone anteflexion in the plane of the scapula
- Prone row with external rotation
- External rotation with Thera-tubing (standing position)
- Horizontal abduction with Thera-tubing (standing position)
- Rows with Thera-tubing (standing position)
- Elevation in the plane of the scapula (standing position)
- Scapula settings
- Scapular protraction and retraction
- Joint mobilization may be included with inferior, anterior, and posterior glides in the scapular plane.
- Stretching exercises should be done by repeating the exercise 3 times and holding the stretch each time for 30 seconds.
Neuromuscular control exercises also may be initiated. PNF patterns will increase strength in rotator cuff muscles and increase the stability of the shoulder. We can use four different patterns.
Modalities that also may be used as an adjunct include cryotherapy, hyperthermia, transcutaneous electrical nerve stimulation, and ultrasound. Intensive ultrasound therapy has been shown to increase calcium resorption, but this requires frequent treatment that may not always be practical.
Self-exercise
- Patient’s starting position: sitting, arm abducted to a position before symptoms appear, contact with three fingertips of the left hand in the supraspinous fossa.
- Movement: pressure into the supraspinous fossa, active adduction of the right glenohumeral joint, then releasing the pressure into the supraspinous fossa, and back to the starting position.
Patients suffering from non-calcifying supraspinatus tendinopathy may benefit from low-energy extracorporeal shock wave therapy, at least in the short term. At the end of the therapy, you should initiate plyometric and sports-specific exercises.
Patient education is again reemphasized, maintaining proper mechanics, strength, and flexibility, and having a good understanding of the pathology. The patient should also show an understanding of a home exercise program with the proper warm-up and strengthening techniques.
How to Prevent Supraspinatus Tendinosis – General Advice
Preventing supraspinatus tendinosis from happening may not be 100% possible if you have a genetic predisposition to tendon degeneration. Age-related wear and tear in the rotator cuff are also normal and expected, especially if you’re over 40.
However, there are some proactive approaches you can take to reduce your risk of supraspinatus tendinosis. The advice below is helpful for non-athletes and athletes alike.
- Practice Regular Shoulder Conditioning: One of the best steps you can take to protect your shoulders from supraspinatus tendinosis is to perform strength training and flexibility exercises (i.e., dynamic and static stretches) on a regular basis. Regularly training and stretching your shoulder and the muscles and tendons surrounding it will help to keep it in optimal shape. (You’ll also keep your shoulder in condition, avoiding “weekend warrior” injuries that happen when you suddenly overtax or overload an under-trained or cold muscle.)
A proper shoulder regimen will strengthen the muscles surrounding and supporting your shoulder, which keeps your mechanics in proper alignment while taking the stress off your tendons. It’s advisable to work with a doctor or physical therapist to design a shoulder conditioning program that works for you. Usually, such a program will target muscle groups that support the shoulder and its rotation: e.g., the upper back, the chest, the biceps and triceps of the upper arm, the shoulder joint itself, and the front of the shoulder. A similar program is often advised for recovery from rotator cuff injuries and surgery, as well.
- Work the Upper Body into Your Exercise Routine: Any form of exercise that strengthens and stretches the upper body—particularly the back and chest—will help to stabilize the shoulder and compensate for heavy use. If you’re not already working upper body muscles as part of your exercise routine, consider adding in an activity that does work those muscle groups: for example, rowing, a dance class, yoga, Pilates, or a cardio weights workout video or class at the gym.
- Maintain Good Posture: Many problems in the body can be caused or made worse by improper alignment, be it when you’re standing, moving around, sitting, or sleeping. Deviating from a neutral posture can put too much stress on a given muscle, ligament, or tendon. This stress can lead to injury. For example, slumped shoulders or lifting your arms to type on keyboards that aren’t ergonomically correct can lead to shoulder pain (and neck pain, and arm pain). Sleeping on one shoulder all night long can also be problematic for shoulder joints.
If you find yourself slumping when you sit or stand, try to make small corrections to your posture—chin up, shoulders back, arms relaxed. If you sleep in a way that hurts your shoulder, consider changing sleep position, using a body pillow, or looking at a mattress that better suits you. At work or at home, take frequent breaks from sitting at a computer or resting in a chair. Get up, walk around, and do some gentle arm, shoulder, chest, and neck stretches.
- Stay at a Healthy Weight: Studies show that being overweight or obese is associated with tendon disease and injuries. Lowering your BMI may help to protect you from tendon degeneration. Preventing or treating diabetes can also cut your risk; poor glycemic control can contribute to inflammation, which can weaken tendons.
- Avoid Lifting, Catching Heavy Objects, or Raising Your Arms Repeatedly: Lifting heavy items over your head or catching them can lead to tendon strain and injury. Try to minimize how often you participate in these activities. (Easier said than done for athletes who practice competitive cheer, competitive pair skating, ballet, or circus arts!) If your occupation requires you to reach over your head for sustained periods (for example, if you paint houses or work in construction), take frequent breaks and ice your shoulder if it’s sore.
- Prevent Falls and Collisions: Practice safety measures to prevent falling onto your shoulder or colliding with people or objects that may push your shoulder ball outside its socket. If you play a contact sport like football, hockey, or soccer, be aware that collisions and falls carry the risk of rotator cuff injury, among other shoulder injuries (like dislocations and tears). Likewise for baseball slides. If you’re older, take extra care to avoid slips and falls.
Supraspinatus Tendinopathy Prevention – For Athletes
The most common recommendation to avoid tendon disease is: don’t overdo it. Avoid overtraining and repetitive strain. For competitive athletes like baseball players, this advice is often difficult to hear and even more difficult to follow. How can you avoid using your shoulder muscles during a normal sports season?
For athletes and others who participate in a shoulder-reliant physical activity daily, there’s no way to completely avoid risk. However, you can avoid putting excess force or strain on the rotator cuff by practicing a few basic measures:
- Work out regularly: Don’t become a weekend warrior; they get hurt more often than athletes who regularly work their bodies and keep them in good condition.
- Work out properly: Know your correct form. Use equipment safely and properly, and make sure all your gear is in good shape. Tennis rackets, for example, need to be properly strung to maintain adequate tension. Shoulder pads and other protective gear should be checked to make sure they fit your body and are still in good working condition.
- Train early (and often): Showing up cold on the first day of your sports season is a certain recipe for injury. Get in shape before your season begins—at least three weeks early, though months before is better.
- Warm up, cool down, and stretch: Don’t skip these critical parts of your workout. Warming up gets the blood flowing to your muscles and tendons, making them more supple and resilient. Cooling down and stretching prevents tightness (tight muscles and tendons can be more prone to tearing and rupture). Both activities maintain and improve your range of motion, which is crucial when relying on a rotating joint like the shoulder—especially if you’re involved in a throwing sport.
- See a professional: For elite athletes, working with a physical therapist or orthopedist is also a smart move. A professional can design a preventative care program for you that will help to keep your rotator cuff—and your entire shoulder joint—as healthy as possible throughout your season. He or she may prescribe exercises to correct alignment and mechanical issues that could contribute to stress and injury. They may also suggest taking NSAIDs to combat tendon inflammation.
The bottom line is that tendinopathy of the shoulder cannot be totally avoided for professional athletes, but you can mitigate your risk by taking care of yourself.
The Clinical Bottom Line
Supraspinatus tendinosis or tendinopathy is a common source of shoulder pain in athletes that participate in overhead sports (handball, volleyball, tennis, baseball).
This tendinopathy or tendinosis is in most cases caused by an impingement of the supraspinatus tendon on the acromion as it passes between the acromion and the humeral head.
Pain and a decrease in range of motion, strength, and functionality are the main complaints that accompany this injury and should be addressed in physical therapy.
There is enough evidence to prove that physical applications such as ultrasound, cryotherapy, hyperthermia, transcutaneous electrical nerve stimulation, and extracorporeal shock wave therapy have a beneficial effect on the recovery of supraspinatus tendinopathy.
But we have to remember that it is very important to use these methods as an adjunct to physical therapy (increasing ROM, strength training of the rotator cuff muscles, and other shoulder stabilizers).
All right, guys, that is it for now for supraspinatus tendinosis. I hope Healthsoothe answered any questions you had concerning supraspinatus tendinosis.
Feel free to contact us at [email protected] if you have further questions to ask or if there’s anything you want to contribute or correct to this article. And don’t worry, Healthsoothe doesn’t bite.
You can always check our FAQs section below to know more about supraspinatus tendinosis. And always remember that Healthsoothe is one of the best health sites out there that genuinely cares for you. So, anytime, you need trustworthy answers to any of your health-related questions, come straight to us, and we will solve your problem(s) for you.
[bwla_faq faq_topics=”frequently-asked-questions-related-to-supraspinatus-tendinosis” sbox=”1″ paginate=”1″ pag_limit=”5″ list=”1″ /]