The year 2020 was a disaster for global health as coronavirus swept the globe. It quickly established itself as one of the world’s leading killers and exposed many healthcare shortcomings. Today, health systems across the globe are battling COVID-19 while also providing critical care to people.
What are those challenges that could be threatening the global health system, you ask? Let’s explore them along with probable solutions.
All of the health issues on the list are urgent, and many of them are interconnected. Each challenge necessitates a collaborative approach from the global health industry, international agencies, legislators, and communities. Without further ado, let’s have a look:
1. Climate Change
According to the WHO, the global climate catastrophe has enormous health effects. Air pollution alone takes the lives of an estimated seven million people each year. Furthermore, the same emissions that cause global warming are responsible for more than 25% of fatalities from chronic respiratory illness, stroke, heart attack, and lung cancer. Climate change has exacerbated malnutrition and has promoted the spread of infectious diseases.
WHO has stated that it is developing “a range of policy alternatives for governments” to reduce the health risks connected with air pollution. To handle the climate crisis, leaders in the public and private sectors must work together to help clean up the environment and prevent further health implications.
2. The Pandemics
Pandemics are characterized as global disease outbreaks. COVID-19 is a typical example of a pandemic, which illustrates our vulnerability to widespread infections. This virus has made healthcare experts realize the importance of global health, compelling them to learn more about it. Now, healthcare professionals are pursuing masters of healthcare leadership online to battle such challenges.
Every year, there are new pandemic risks to contend with, unfortunately. Vaccination initiatives can assist, but it’s also necessary to address the problems at the root, such as health education and ethical agricultural practices. Researchers have also provided proposals for global risk mitigation policies.
3. Healthcare Equity
There are significant differences in the quality of people’s health across socioeconomic classes. According to WHO, there is an 18-year disparity in life expectancy between individuals in low- and high-income nations. Furthermore, there exist significant differences in life expectancy in individuals within the same cities and countries.
Cancer, diabetes, and other non-communicable diseases strain people belonging to low- to middle-class households. WHO stated it is working to enhance child and maternity care, nutrition, gender equality, mental health concerns, and access to drinkable water and sanitation worldwide. It’s also working on a plan regarding how nations should work together to increase healthcare equity. To address these economic obstacles, global health professionals must look for ways to include underrepresented communities in public health discussions. They must encourage physicians to practice in rural areas and implement policies that advance healthcare access and lower barriers.
4. Access to Treatments
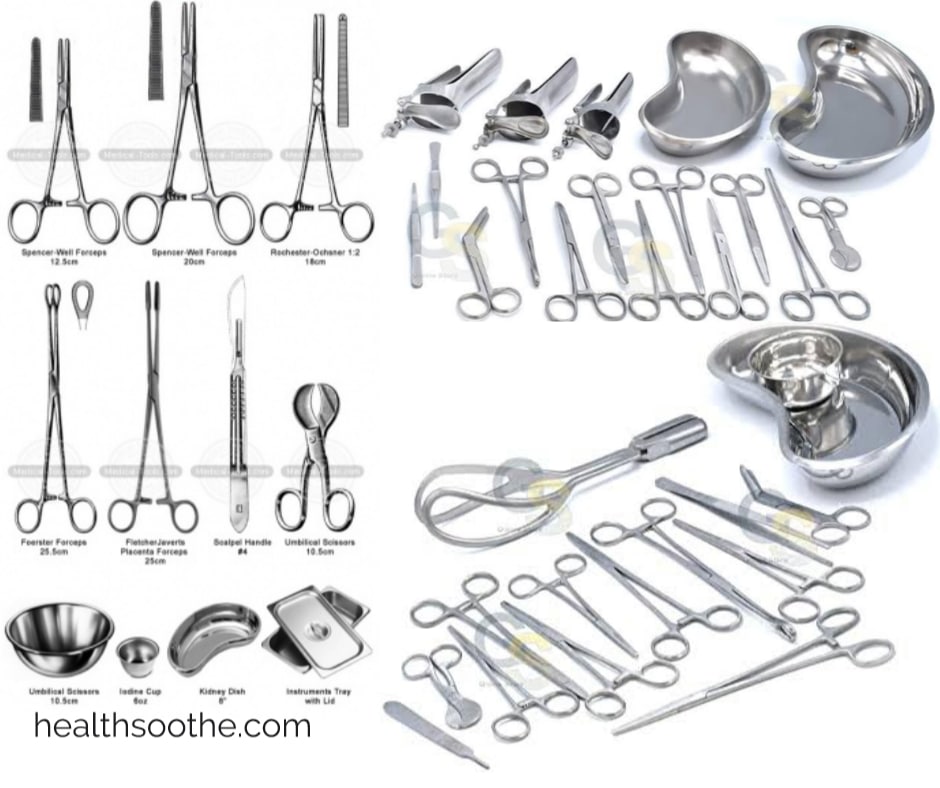
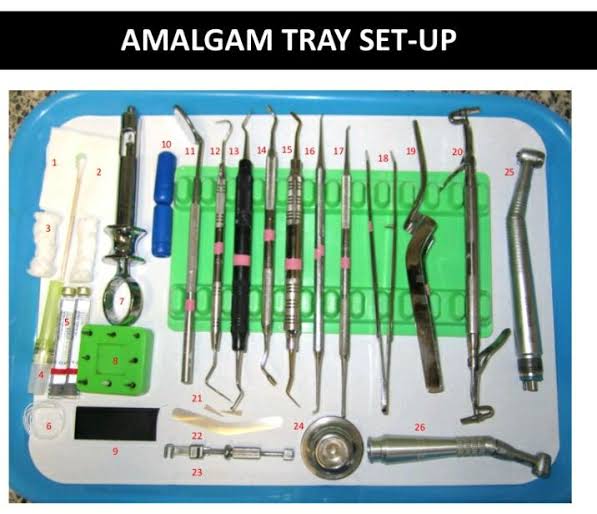
According to WHO, one-third of the world’s population lacks access to essential health items such as diagnostic equipment, medicines, and vaccines. Limited access to these items fuels drug resistance and puts people’s lives and health at risk.
Authorities must “hone in” on efforts to combat substandard and falsified medical products to address the problem. There is also a need to strengthen the capacity of developing countries to ensure the quality of medical products throughout the supply chain. Likewise, improving access to diagnosis and treatment of non-communicable diseases (NCDs) is also critical.
Education can help people recognize and improve lifestyle variables such as poor diets, inactivity, smoking, and alcohol abuse, which can significantly cause these diseases.
5. Preparing for Epidemics
A pandemic caused by an airborne, highly infectious virus is “inevitable.” Still, countries throughout the world continue to spend more money responding to disasters than planning for them. It leaves countries unprepared for the next pandemic, which might risk the lives of millions of people.
The COVID pandemic has taught us that countries should use evidence-based methods to strengthen their health systems. And safeguard people from disease outbreaks, natural disasters, and other health emergencies.
6. Resistance to Drugs
Antimicrobial resistance (AMR) is growing around the world. Antimicrobial resistance can quickly spread across borders and continents due to the modern mobility of people, animals, and commerce.
It is a public health priority to combat this menace. To detect, prevent, and respond to these dangers when they occur. The AMR Challenge led to the One Health approach, emphasizing that human health intertwines with animal and environmental health. This approach elicits professionals from human, animal, environmental, and other relevant disciplines/sectors to monitor and control public health concerns. It also entails learning about how illnesses spread among plants, humans, animals, and the environment.
Efforts to eradicate infectious diseases globally will only be successful if we have effective medicines to treat them. So, to preserve antimicrobials, it will be critical to continue working with healthcare partners. These include the Food and Agriculture Organization, the World Organization for Animal Health, and other stakeholders.
7. Improving Public Trust in Health Workers
The spread of misinformation, combined with a lack of trust in public institutions, is playing an increasingly important role in the health decisions of the public. Patients who trust healthcare systems are more likely to accept the recommendations of healthcare workers on how to rely on healthcare services and make healthy choices.
WHO is trying to help countries “strengthen their primary care.” It is battling disinformation on social media platforms to boost public trust in healthcare providers and institutions. Scientists and the public health community also need to better listen to the communities they serve.
8. Sanitization Concerns
Billions of people worldwide live in communities without appropriate sanitation or drinking water, both of which can spread diseases. Roughly a quarter of healthcare institutions in developing nations lack essential water services, crucial to healthcare systems. Lack of water and other necessary resources results in poor-quality care and raises the risk of illness.
Thus, to address this concern, there is a need to work with developing nations. Such efforts can help enhance hygiene, sanitation and improve water conditions in healthcare institutions to address the problem.
Conclusion
The ever-growing list of global health challenges can be daunting. Still, there are several ways we, as individuals, can make a difference. A small effort can add up quickly if enough individuals join the cause.
The global health community can gradually strengthen the global health system through national, regional, and international activities. It is possible if all countries unite to resolve and achieve universal health coverage and global health security.




Covid 19 put a bad impact on people’s health all across the globe. However, efforts have been made to overcome its impact and we have seen many solutions like vaccines to save people’s lives. Also, there is a huge preference for telehealth solutions to get treatment to minimize contact with other people.