Most people envisage ink poisoning as someone ingesting ink, and they are right to some extent. If you've ingested ink, such as by biting on the base of a pen and putting ink in your mouth, you shouldn't be too worried if you swallowed a little.
Quick Facts About Ink Poisoning
| A | B |
|---|---|
| Definition | Ink poisoning refers to the harmful effects caused by exposure to ink or ink ingredients |
| Possibility | Ink poisoning is rare and usually occurs when large quantities of ink are ingested |
| Symptoms | Symptoms may include stained skin or tongue, mild stomach upset, nausea, vomiting, headache, skin irritation, dizziness, blurred vision, allergic reactions |
| Causes | Ingestion, inhalation, or absorption of ink through the skin |
| Toxicity | Depends on the type of ink and the amount ingested or absorbed. Some inks contain toxic chemicals |
| Treatment | Drinking water is suggested if ink is swallowed; Immediate medical attention is needed for large amounts. Treatment may involve supportive care and symptom management |
| Prevention | Keep ink away from children, avoid ingesting ink and ensure tattoo equipment and ink are sterile, handle with care, avoid prolonged exposure, and ensure proper ventilation |
| Long-Term Effects | Chronic exposure to certain ink chemicals may lead to serious health issues |
Ink poisoning only occurs when you have ingested ink into your body in large quantities. In today’s article, we aim to explain all there is to know about ink poisoning – what is its symptoms and causes? We will also explain how to treat and prevent ink poisoning, as well as other key things you need to know about ink poisoning.
We move!
What is Ink Poisoning?

Ink poisoning occurs when someone swallows large quantities of ink found in writing instruments (pens). Skin/eye contact may also result in exposure which also can lead to ink poisoning.
Want an audio-visual explanation, watch the video below:
So, What is in Writing Ink that Causes Ink Poisoning?
In other words, what are the constituents or ingredients of writing ink that leads to ink poisoning when the ink is swallowed? What causes ink poisoning? Writing ink is a blend of dyes1Pen or marker ink. (2019). illinoispoisoncenter org, pigments, solvents, and water.
Writing ink is typically thought to be nonpoisonous2medlineplus gov. The individual may not need hospitalization.
Tattoo ink toxicity has received minimal attention, and ink makers are not required to reveal the specific ingredients of their products. As per published studies, some inks include pigments used for printer toner or automobile paint.
The Food and Drug Administration (FDA) in the United States has not authorized any pigments for cosmetic injection into the skin. The FDA is also receiving complaints of patients getting infections from tainted tattoo inks, along with bad reactions towards the inks themselves.
Hundreds of unwanted outcome reports involving tattoos have been received by the FDA throughout the years. There is no foolproof method to know whether tattoo ink is harmless. Even though the containing vessel is sealed and the label states that the product is sterile, tattoo ink might get contaminated.
Infections as well as allergic reactions have been linked to "do-it-yourself" inks as well as kits sold to consumers. The FDA is also worried that consumers may be unaware of how to regulate and avoid all potential sources of contamination.
Between 1984 and 1989, 31 Sudanese children were hospitalized due to para-phenylenediamine and henna dye poisoning. There was a typical clinical presentation. All of the children had severe and acute angioneurotic edema, and 15 of them needed an emergency tracheostomy due to breathing obstruction.
5 children that recovered from peritoneal dialysis had acute renal failure. All 13 fatalities occurred within 24 hours after presentation, indicating a high rate of mortality. A bad prognosis was given by hypotensive shock.
Similar incidences may be happening unnoticed in areas where henna is routinely used. Intake was accidental in 12 instances, purposeful in ten, and homicidal in three. In the remaining six, cutaneous absorption was most probable.
What are the Symptoms of Ink Poisoning?

The ink from highlighters, markers, pens, and other similar items is regarded as mildly harmful and in such tiny quantities that it is seldom a cause for worry. Symptoms include discolored skin, tongue, and albeit uncommon, slight stomach distress.
Because of the volume of ink in stamp pads and printer cartridges, if ink from one of these sources has been ingested, seek medical assistance.
Other symptoms include:
- Eye irritation
- Vomiting
- Staining of skin and mucous membranes
- Headaches
- Nausea
- Consuming large quantities of ink, particularly printer ink, may cause severe central nervous system symptoms.
You may get a rash— bumps or redness —in the location of your tattoo, as well as a fever.
More serious infections might produce a high temperature, shaking, chills, and sweating. Such infections may need a long course of antibiotics, sometimes for months, as well as hospitalization and/or surgery.
A rash might potentially indicate an allergic response. Furthermore, since the inks are irreversible, the response may last. Should you have any concerns, consult with your doctor.
After getting a tattoo, you may acquire scar tissue, or you may get "granulomas," which are little knots or lumps that grow surrounding the material which the body recognizes as alien. If you are prone to keloids (scars that expand beyond their usual bounds), you may have a similar response to the tattoo.
Some individuals may experience burning or swelling in their tattoos during MRI, although this is uncommon and does not persist long. Before having an MRI, inform your healthcare provider that you've got a tattoo3Skerrett PJ. (2012). Tattoos and infection: Think before you ink. health harvard edu.
Ink Poisoning Due to Ink on Skin

Drawing on the skin does not cause ink poisoning. Ink may stain your skin briefly, but it isn't going to poison you.
Ink Poisoning Due to Ink in Your Eye

Eye discomfort from the ink is more prevalent than skin irritation. If you suspect you have ink in the eye, rinse it with lukewarm water until the irritation subsides.
Although ink in your eye may temporarily discolor the white area of your eye, it is unlikely to create permanent or long-term issues. Consult your doctor if the discomfort persists or you have impaired vision.
Tattoos and Ink poisoning

Based on a 2015 study of 2,225 United States adults, 29% had at least one tattoo, and 69 percent had two or moreTattoo takeover: Three in ten Americans have tattoos, and most don't stop at just one. (2016). According to the United States Food and Drug Administration (FDA), while getting a tattoo, you should be on the alert for unsanitary methods and equipment that hasn't been disinfected4Management of Poisoning - A Handbook for Health Care Workers. (1997). helid digicollection org, but ink should also be a worry5Mayo Clinic Staff. (2018). Tattoos: Understand risks and precautions. kcms-prod-mcorg mayo edu/.
Infections may occur when tattoo ink or color is infected with mold or bacteria. The FDA classifies tattoo ink as a cosmetic product. There are no FDA-approved pigments (coloring chemicals) for injecting into the skin for cosmetic reasons.
Infection and Adverse Response to Tattoos
You may experience rashes in the region after having a tattoo. An allergic response or an infection might be the cause. The pigments more likely to trigger allergic skin responses are: red, yellow, green, and blue.
Symptoms of an aggressive infection may include high temperature, sweats, chills, and shakes. Antibiotics are normally used to treat infected tattoos; however, hospitalization or surgery may be required.
What Ought to be Done if You have an Allergic Response to Tattoo Ink?
The very first step is to consult with your doctor about a diagnosis and treatment plan. The diagnostic might identify whether the response is caused by the ink or by other factors such as unsanitary application.
Your next step should be to speak with the tattooist for two reasons:
- Your doctor may want information about the ink, such as the color, brand, and batch number.
- Your tattooist is going to trace the ink so that it is not reused.
Discuss with your doctor the possibility of reporting the occurrence to the FDA so that safety information may be updated and distributed.
Can Ink Poisoning Kill?

Ink poisoning can only lead to fatal complications when consumed in large quantities, and if immediate treatment isn't rendered to the person within a period of 3-12hrs , sometimes even more than that (even days) depending on how much volume of ink the person consumed.
And the only time ink poisoning can be fatal is only the ink was drank, but apart from that, ink poisoning that could come from the skin being in contact with ink and leading to adverse reactions; this type of ink poisoning isn't fatal. But, if left untreated, it could lead to serious skin infections, and there is a possibility of tetanus also occurring due to the infected area left untreated and open for a long while.
Ink poisoning due to ink in the eye isn't also fatal, but this type of ink poisoning is dangerous, and lead to serious complications like permanent eye problems, even to the extent of losing that eye, if left untreated for long.
If you are undergoing ink poisoning, or someone you know has been ink poisoned, get medical attention straight away. Do not force someone to vomit unless instructed to do so by a poison control center or even a health care expert.
Note: Before ink poisoning reaches a fatal level, large volumes of writing ink (over an ounce or 30ml) must be ingested.
How Do You Treat Ink Poisoning?
If you are undergoing ink poisoning, or someone you know has been ink poisoned, get medical attention straight away. Do not force someone to vomit unless instructed to do so by a poison control center or even a health care expert.
Before therapy is required, large volumes of writing ink (over an ounce or 30ml) must be ingested.
Home Care
Get medical help right away. Do not make a person throw up unless told to do so by the poison center or a healthcare professional.
Note: Large amounts of writing ink must be consumed (more than an ounce or 30 milliliters) before treatment is needed.
Before Calling the Emergency Care Number
Get the following information:
- Person's age, weight, and condition
- Name of the product (and ingredients and strengths, if known)
- Time it was swallowed
- Amount swallowed
- Poison Control
Your local poison control center can be reached directly by calling the national toll-free Poison Help hotline (1-800-222-1222) from anywhere in the United States or the emergency response number of your area.. This national hotline will let you talk to experts in poisoning. They will give you further instructions.
This is a free and confidential service. All local poison control centers in the United States use this national number. You should call if you have any questions about poisoning or poison prevention. It does not need to be an emergency. You can call for any reason, 24 hours a day, 7 days a week.
There are mainly 4 treatments used to treat ink poisoning;
1. Lavage of the stomach

In most cases, gastric lavage is preferred to ipecac administration, especially in emergency rooms where extended ipecac-induced puking may prolong treatment using activated charcoal.
Ingestions of very poisonous compounds (large ingestions or substances linked with significant morbidity and/or mortality); substances not adequately absorbed by activated charcoal (i.e., lithium, iron, lead, methanol); and individuals with the potential for a compromised airway are all indications for lavage (e.g., altered alertness).
Consumption of corrosives and also most hydrocarbons (gastric evacuation is indicated after intakes of products containing hydrocarbons like benzene, toluene, camphor, halogenated hydrocarbons, pesticides, or heavy metals, or if the intake was larger than four to five mL per kg); patients having depressed gag reflexes who are not intubated; and clinically insignificant ingestions are all contraindications to gastric lavage.
Aspiration and esophageal or bronchial perforation are two complications. A 28- to 36-inch French tube is appropriate for toddlers; a 36- to 40-inch French tube is appropriate for adults 8).
In children, gastric lavage is performed using tap water or normal saline in 15mL/kg aliquots until clean. Adults’ lavage with 300mL aliquots till clear, up to 10-20 L if necessary. In patients having potentially lethal ingestions, administering activated charcoal via the lavage tube both before/after lavage may be advantageous.
2. Ipecac

Ipecac is still beneficial in the phone treatment of alert patients who are unable to go to a health care institution within one hour of consumption. Ipecac administered at home by skilled hospital professionals treating kid poisonings after ingestions assessed as not being "high-risk" has been found to reduce pediatric/child emergency department visits without affecting safety.
Ipecac syrup is given in the following dosages: 10 mL for babies six months to one-year-old, 15 mL for children one to twelve years old, and 30 mL for teenagers over twelve years old.
To improve the effectiveness of stomach emptying with emesis, water is taken immediately after the ipecac; adults should get 8-16oz; children should have 4 to 8 oz; and infants under 1 year of age should receive 5-15 mL per kg body weight.
Children under the age of six months, patients that are already puking, patients with changed mental state or impaired gag reflexes, including patients who have eaten drugs that produce seizures or diminished responsiveness should not be administered ipecac.
Ipecac should not be used after ingesting corrosives (alkalis or acids), sharp objects, or many hydrocarbons (akin to gastric lavage), or when therapy with activated charcoal is expected within 60 to 90 minutes.
3. Activated Charcoal

When administered alone or after gastric emptying, activated charcoal is the backbone of gastric cleansing and is useful for most oral poisonings. Caustic acids, alkalis, alcohols, lithium, and heavy metals are exceptions (e.g., iron, arsenic). Activated charcoal remains inert and persists throughout the gastrointestinal system, providing a vast surface area for toxin adsorption.
Furthermore, activated charcoal may reduce the absorption of medicines that pass via the enterohepatic or enterogastric circulation. For both children and adults, the normal dosage is 1-2 g/kilogram, administered as a single dose in conjunction with a cathartic.
To make a slurry, the charcoal is combined with water in a 1:4 to 1:8 ratio (1 part charcoal to 4 or 8 parts water); minor amounts of fruit juice or cocoa powder might enhance the flavor. Multiple doses (1 g per kg every two to six hours) have been demonstrated to be effective for carbamazepine, phenytoin (Dilantin), phenobarbital (Tegretol), theophylline, digitalis, salicylates, and dapsone poisonings.
When using repeated dosage, a cathartic may be given with the first dose but should not be given with subsequent doses due to the risk of significant fluid and electrolyte abnormalities. Mechanical intestinal blockage and ileus are both contraindications to using activated charcoal.
4. Irrigation of the whole bowel
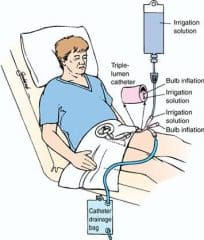
Isosmotic cathartic solutions are used in whole-bowel irrigation to flush and cleanse the intestines. It may be useful in individuals who have consumed chemicals that are not effectively absorbed by activated charcoal and/or are not susceptible to lavage.
Iron, lithium, and slow-release potassium are examples of such compounds, as are packets or vials containing cocaine and other narcotics. Irrigants (Golytely, Colyte) often used include a polyethylene glycol electrolyte solution that is not absorbed via the gastrointestinal system and does not create substantial fluid or electrolyte imbalances.
The solution is given orally or through a nasogastric tube at a rate of 2 L per hour for adults and 0.5 L per hour (or 25 to 40 mL per kg per hour) for children until the rectal effluent is clear.
Individuals tolerate the operation best when they are aware and seated on a commode; supine patients benefit from the placement of a rectal tube. Mechanical blockage, ileus, perforation, and gastrointestinal hemorrhage are all contraindications to whole bowel irrigation.
What to Expect at the Emergency Room
The healthcare provider will measure and monitor the person's vital signs, including temperature, pulse, breathing rate, and blood pressure. Symptoms will be treated as appropriate. The provider may wash the person's eyes or skin to remove the ink.
Note: The person may not need to be treated in a hospital.
Could More Issues Arise in the Future Due to Ink Poisoning?
Although study at the FDA and elsewhere is underway, there are many unanswered issues concerning the long-term consequences of pigments, other components, and toxic elements in tattoo inks6Think before you ink: Are tattoos safe? (2017). fda.gov/consumers/consumer-updates/think-you-ink-are-tattoos-safe.
The FDA has collected reports of adverse responses to tattoo inks both immediately after tattooing and years later. If your tattoo includes p-phenylenediamine, you may potentially develop an allergy to other items, such as hair colors (PPD).
There's also tattoo removal. Scientists are unsure of the short- and long-term repercussions of how pigments degrade following laser therapy. They are aware, however, that certain tattoo removal techniques may result in permanent scars.
Remember that tattoo removal is a time-consuming operation, and full removal without scars may be difficult.
Additional resources and citations
- 1Pen or marker ink. (2019). illinoispoisoncenter org
- 2medlineplus gov
- 3Skerrett PJ. (2012). Tattoos and infection: Think before you ink. health harvard edu
- 4Management of Poisoning - A Handbook for Health Care Workers. (1997). helid digicollection org
- 5Mayo Clinic Staff. (2018). Tattoos: Understand risks and precautions. kcms-prod-mcorg mayo edu/
- 6Think before you ink: Are tattoos safe? (2017). fda.gov/consumers/consumer-updates/think-you-ink-are-tattoos-safe
The content is intended to augment, not replace, information provided by your clinician. It is not intended nor implied to be a substitute for professional medical advice. Reading this information does not create or replace a doctor-patient relationship or consultation. If required, please contact your doctor or other health care provider to assist you to interpret any of this information, or in applying the information to your individual needs.