Defining/Explaining Peak Inspiratory Pressure (PIP)
[ninja_tables id=”73411″]
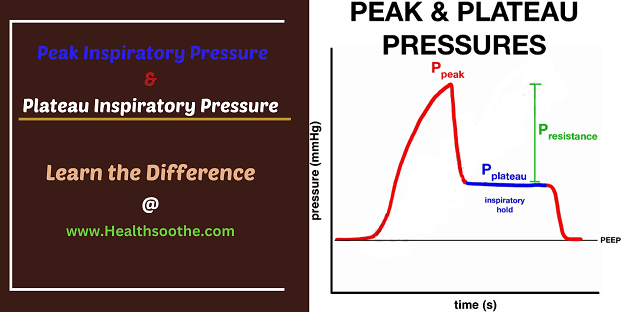
Peak inspiratory pressure is the pressure that is generated by the ventilator to overcome both airway resistance and alveolar resistance. The goal of the pressure is to obtain the set inspiratory flow and the tidal volume goal that is set by the provider.
The maximum amount of pressure exerted in the lungs while inhaling is known as peak inspiratory pressure (PIP).[mfn]https://www.sciencedirect.com/topics/nursing-and-health-professions/peak-inspiratory-pressure[/mfn] The number in mechanical ventilation represents a positive pressure which is in centimeters of water pressure (cmH2O).
It is frequently referred to as the maximum inspiratory pressure (MIPO) in normal breathing, which is a negative number.
Peak inspiratory pressure rises in the presence of airway restriction. PIP may be raised by increased secretions, bronchospasm, chewing on ventilation tubing, and impaired lung compliance.
Except if the individual experiences acute respiratory distress syndrome, the PIP should never be continuously greater than 40(cmH2O).
The formula for peak pressure with a square waveform is:
Peak inspiratory pressure = (Resistance x Flow) + (Elastance of respiratory system x Tidal volume) + PEEP
Hence, if any of these variables increase for reasons that we will discuss below, the peak pressure will go up. Keep in mind that you’ll never need to calculate this or use a ventilator maneuver to obtain this number. This number is seen on the ventilator.
Plateau pressure: This is the pressure that is essentially left over in the lungs after the tidal volume has been delivered.
Plateau pressure = Tidal Volume/Compliance
Want an audio-visual (video) explanation, if yes, watch the video below:
Measuring the Peak Inspiratory Pressure At zero flow
In order to measure this, an inspiratory hold has to be done on the ventilator. This is where the ventilator pauses for several seconds after the tidal volume has been delivered, which eliminates flow, and thus, airway resistance.
This number is a reflection of the compliance of the lung. If the lung is very compliant as in patients with COPD, the plateau pressure is lower. If the lung is not compliant, as in patients with ARDS or fibrotic lung disease, the plateau pressure will be high.
Differentiating Peak Inspiratory Pressure from Plateau Inspiratory Pressure
Peak Pressure
Peak pressure applies when there is airflow in the circuit, i.e., during inspiration. What determines the peak pressure is the airway resistance in the lungs. So, it follows that if there is a problem with the airways the peak pressure will rise.[mfn]https://en.wikipedia.org/wiki/Peak_inspiratory_pressure[/mfn]
Plateau Pressure
Plateau pressure applies when there is no airflow in the circuit. That is when inspiration is complete. This pressure is determined by lung compliance. So, it follows that if there is a problem with compliance, the plateau pressure will rise.
So, let’s work through this diagram to help our understanding of the difference, and how it can help us interpret the information.

If we ventilate the lung then the airway pressure will go up and the flow will increase (1).
When we release the breath, the pressure will go down, and the flow will move in the opposite direction as the air moves out (2). The flow then returns to baseline (3).
Let us then say that we inflate the lungs but then hold them at inflation for a period of time. The pressure will reach a peak (4), and then as the breath-hold comes in there will be an equilibrium pressure (5), (remember the balloon analogy here: it takes high pressure to inflate the balloon, but once inflated, a lot less effort to keep it inflated) until the release of the pressure as exhalation takes place (6).
You can see on the flow line the period between (5) and (6) where there is no flow as the breath-hold takes place.
So, remember, peak pressure (circled) is a reflection of the airways, and plateau pressure is a reflection of lung compliance.
Remembering that important fact, let’s look at a couple of examples that we might encounter.
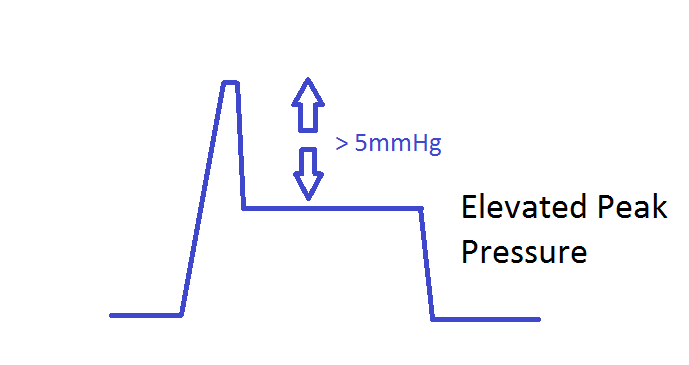
So firstly, we can look at a waveform demonstrating a high peak pressure.
If the difference between the peak pressure and the plateau pressure is greater than 5 mm Hg then which is defined as an elevated peak pressure.
The other extreme would be where there is not a problem with the peak pressure but instead with a high plateau pressure.
So, if the pressure alarm is going off you need to know whether it is a high peak pressure causing the problem or a high plateau pressure.

Elevations in the Peak and Plateau Pressures:
High Peak/Normal Plateau: issue with elevated resistance

There is resistance in the ETT or distal bronchus, which decreases the diameter and thus requires the ventilator to increase pressure to achieve the same desired tidal breath. Below are common issues with isolated high peak pressures and solutions to these issues.
- Kink in the circuit: examine ventilator tubing
- Fluid accumulation: clear the fluid from the circuit
- Biting the ETT: increase sedation or insert bite block
- A small ETT with biofilm-forming: consider changing out the tube
- High flow rate or tidal volume: adjust ventilator settings
- Ventilatory asynchrony: increase sedation
- Laryngospasm or bronchospasm: consider steroids, epinephrine
- Mucous plugging: clear out ETT
- Foreign body: removal
High Peak and high plateau pressures: Issues with Compliance

For the reasons stated below, there may be an issue with low compliance of the lungs, which forces the ventilator to have an increase in pressure.
- Pneumonia: if this has been gradually worsening, consider ventilator-associated pneumonia. Obtain chest x-ray, respiratory cultures, and start broad-spectrum antibiotics
- Pulmonary edema: Consider diuresing and adjusting PEEP
- Auto PEEP: this is seen in breath stacking where the patient does not have a full exhalation. It is common in COPD and reactive airway diseases. Adjust the PEEP, tidal volumes, or inspiratory: expiratory time ratio. Consider sedation as well. If very severe, this can be immediately corrected by removing the patient from the ventilator (and manually ventilating), while allowing the air to leave the circuit.
- Right main stem intubation: retract endotracheal tube
- Pneumothorax: This should be considered with sudden onset hypoxia and hypotension. Evaluate with ultrasound and/or chest x-ray. Resolution is attained with decompression and chest tube placement.
- Atelectasis, pulmonary fibrosis and even abdominal issues like abdominal compartment syndrome can increase the plateau pressures.
Why is Peak Inspiratory Pressure (PIP) important?
Because a high peak pressure is an airway issue, for example:
- Bronchospasm
- Retained secretions
- Mucous plug
- ETT tip occlusion
…and a high plateau pressure is a compliance issue, for example:
- Pneumothorax
- Pulmonary oedema
- ARDS
- Pneumonia.
So, understanding the difference between peak pressure and plateau pressure will help you diagnose what may be wrong with a patient’s ventilation.
What about Positive End Expiratory Pressure (PEEP) – Mechanical Ventilation
What is PEEP, why do we use it and what are the pros and cons?

As inspiration occurs (1) the alveoli expands to allow the air in. Gas exchange can then take place as the blood supply moves past the wall of the alveoli.
During expiration the alveoli contracts down (2). It does not completely collapse, partly due to the presence of a substance called surfactant (3). This decreases the surface tension within the alveoli ensuring that complete collapse cannot take place.
Unfortunately, ventilation of a patient tends to inactivate the pulmonary surfactant which then leads to the collapse of the alveoli (4), making the gas exchange more difficult as the surface area of the lung is now reduced.
The ventilator also causes an increase in alveolar capillary permeability and causes the activation of inflammatory cells and the release of cytokines
If you want to see what a difference PEEP can make to the inflation of the collapsed alveoli then watch this short video. Initially no PEEP, then the valve is applied.
Effect of PEEP on the Lungs
The consequence of this is that the alveoli are opening and collapsing much more than they would normally and will also be subject to higher pressures in order to reopen them with each breath. This combination will damage the alveoli further.
Positive end-expiratory pressure (PEEP), is a pressure applied by the ventilator at the end of each breath to ensure that the alveoli are not so prone to collapse. This ‘recruits’ the closed alveoli in the sick lung and improves oxygenation.
So, PEEP:
- Reduces trauma to the alveoli
- Improves oxygenation by ‘recruiting’ otherwise closed alveoli, thereby increasing the surface area for gas exchange.
- Increases the functional residual capacity- the reserve in the patients’ lungs between breaths which will also help improve oxygenation.
- Ventilation/perfusion mismatches are improved.
- Increases the compliance of the lung
Compliance is the relationship between the change in volume and the change in pressure in the lung. With PEEP, less pressure is needed to get the same volume of air into the lung as the alveoli are already partially inflated and therefore do not need that high initial pressure to open them. (Remember the balloon analogy- hard to blow up initially, but then much easier to inflate after the initial breath).
Problems with PEEP

PEEP can cause some problems for those patients who have some airway obstruction i.e. Asthmatics, and those with COPD.
If we look at the alveoli of a person with obstructive disease, we can see the obstruction in the airway (3) and the ventilator is blowing air down into the alveoli (1).
Once the ventilator has finished putting air into the lung, expiration is then a passive process, relying on the passive recoil of the chest wall and lung (2).
But because the obstruction is there, this air takes longer to get out of the lung. The ventilator does not wait for the air to come out before it delivers the next breath. This means in the obstructed patient that not all the air will come out of the alveoli before the next breath comes in.
The air that is left over will exert a pressure on the alveolar walls, helping to keep them open (4).
As continued breaths come in the alveoli will become larger, so exerting more pressure on the internal walls of the alveoli (4).
The increased force on the inside tends to then increase the recoil exerted by the lung tissue on the outside of the alveolar wall (5). This increased recoil will help push some more air out of the alveoli past the obstruction.
This process will continue until a steady state is reached, where the amount of air coming in is equal to the amount of air coming out (6).
This balancing of pressure, with the ventilator’s involvement, keeps the alveoli open and is referred to as Auto-PEEP and the lung volumes, which were higher than before, are referred to as Dynamic Hyperinflation.
The phenomenon of not being able to get one breath out of the lung before the next breath comes in is known as Breath Stacking.
The other problem PEEP can cause is a drop in cardiac output. Venous return to the heart is very dependent on the difference in pressure between that in the thoracic cavity (Pt), where the heart is enclosed, and that in the circulatory system (Pet)
VR = Pet – Pt
 PEEP will cause a rise in the intrathoracic pressure, meaning the difference between the two pressures will fall, causing a reduction in the venous return.
PEEP will cause a rise in the intrathoracic pressure, meaning the difference between the two pressures will fall, causing a reduction in the venous return.
The respiratory system in normal breathing is a negative pressure system. The drop in pressure in the thorax causes the air to move in. This drop in pressure also relieves some of the pressure on the right side of the heart allowing it to fill more easily.
By applying PEEP, we are reducing that drop in pressure. The consequence of this is that we also then affect the right side of the heart potentially reducing cardiac output.
The increased pressure in the thoracic cavity also increases the pressure in the pulmonary system, meaning that the right side of the heart has higher pressures to push against to get the blood through the lungs.
This in turn makes the right side become bigger, which then pushes against the left side of the heart which will then reduce cardiac output.
How Much PEEP?
The American Thoracic Society recommends higher rather than lower values of PEEP, but bear in mind the overall aim is to achieve adequate oxygenation without compromising the patient’s cardiac output.
The ARDSnet study also recommends plateau pressures not above 30cm H2O. In my experience, I have not seen PEEPs above 12 cm H20 being applied.
The Debrief
- Peak pressure: This is the pressure that is generated by the ventilator to overcome both airway resistance and alveolar resistance.
- Plateau pressure: This is the pressure that is essentially left over in the lung after the tidal volume has been delivered.
- High Peak pressures and normal plateau indicate an issue with elevated resistance
- High Peak and high plateau pressures indicate an issue with compliance
In volume control ventilation, changes in resistance and compliance cause changes in the measured peak and plateau airway pressures. Once we understand these measurements, we can recognize patterns to diagnose changes in the patient/ventilator system.
All right, guys, that is it for now for peak inspiratory pressure. I hope Healthsoothe answered any questions you had concerning peak inspiratory pressure.
Feel free to contact us at contact@healthsoothe.com if you have further questions to ask or if there’s anything you want to contribute or correct to this article. And don’t worry, Healthsoothe doesn’t bite.
You can always check our FAQs section below to know more about peak inspiratory pressure. And always remember that Healthsoothe is one of the best health sites out there that genuinely cares for you. So, anytime, you need trustworthy answers to any of your health-related questions, come straight to us, and we will solve your problem(s) for you.
[bwla_faq faq_topics=”frequently-asked-questions-associated-with-peak-inspiratory-pressure-pip” sbox=”1″ paginate=”1″ pag_limit=”5″ list=”1″ /]