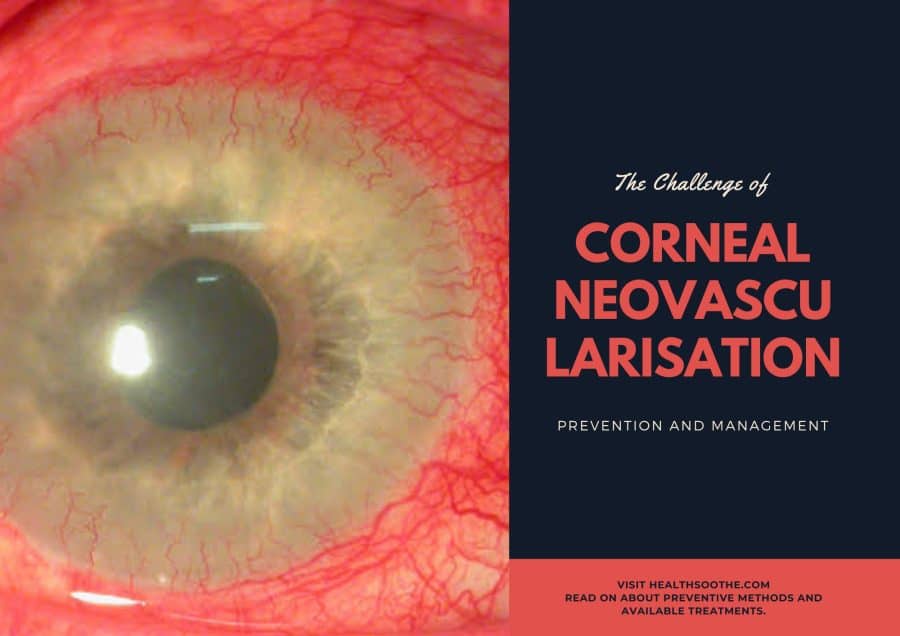
Corneal neovascularisation (CNV) is an eye disorder that is characterized by the growth of new blood vessels in the cornea, leading to impaired or loss of vision. The challenge of corneal neovascularisation is managing and preventing its progression with various treatments. The current treatments available can vary depending on the severity of the disorder. Prevention of CNV is an important step in the management of this disorder, as it can reduce the risk of vision loss and the progression of the disease. While there are various treatments available, understanding the risk factors and prevention of CNV can help reduce the burden of this disorder and improve patient outcomes. In this blog post, we will briefly explore the challenge of corneal neovascularisation, discussing the risk factors, preventive methods, and available treatments.
Read more about CNV and other eye-related disorders.
1. Causes of CNV
Corneal Neovascularisation (CNV) is a condition caused by the growth of new, aberrant blood vessels in the corneal tissue. It is a major challenge in ophthalmology, and can cause significant visual impairment and sometimes even blindness. The primary causes of CNV are prolonged inflammation or injury to the cornea due to a variety of factors, including exposure to ultraviolet radiation, contact lens wear, and ocular trauma. In addition, a variety of systemic disorders, such as diabetes, autoimmune diseases, and HIV, can also increase the risk of CNV by causing inflammation of the cornea. In some cases, CNV can also be caused by certain topical medications.
2. How to Prevent Corneal Neovascularisation
There are both short-term and long-term strategies for CNV prevention. In the short term, the key is to treat the primary cause of the disease through the adequate use of antibiotics and antiviral medications. Additionally, patients should be monitored for any corneal diseases that may be associated with neovascularisation, such as herpes simplex keratitis. Long-term prevention measures include regular eye examinations, proper nutrition [mfn]https://www.healthline.com/nutrition/8-nutrients-for-eyes[/mfn], refraining from contact lens use, and avoiding cigarette smoke and other environmental pollution. Finally, patients should be aware of the signs and symptoms of corneal neovascularisation and seek immediate medical attention if they occur.
3. Managing Corneal Neovascularisation
Managing corneal neovascularisation involves keeping the corneal surface healthy. This includes maintaining good hygiene, using artificial tears or lubricants to help keep the surface moist, and avoiding contact lenses or any contact with foreign objects that could cause trauma or infection. In some cases, it may also be necessary to use medications to reduce inflammation and control the growth of new vessels. Finally, the patient should be monitored regularly to detect any signs of disease progression or recurrence.
In conclusion, corneal neovascularisation is a complex and challenging condition that requires careful management and preventive measures to reduce the risk of vision loss. With the right approach, it is possible to reduce the risk of disease progression and visual impairment, while providing the patient with better quality of life. The key is to seek professional medical help to identify and address the underlying cause of the condition, and spot potential complications. With early diagnosis and appropriate treatment, it is possible to reduce the severity of the disease and improve vision.